Overview of Pilon Fracture Treatment Approaches
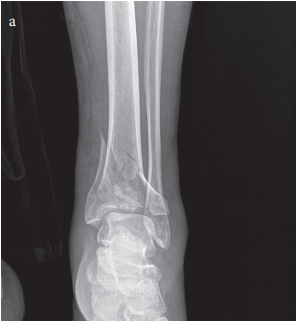
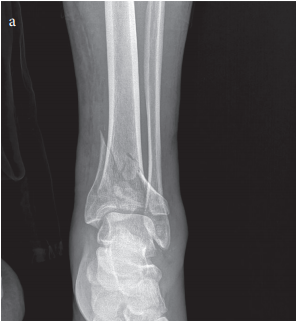
Pilon fractures, involving the distal tibia near the ankle, continue to challenge the field of orthopaedic trauma with their tricky parts and tangled issues. Managing these injuries requires a careful balance between achieving proper bone alignment and preserving the soft tissue envelope – a task many clinicians find both intimidating and nerve-racking. In this opinion editorial, we take a closer look at Minimally Invasive Plate Osteosynthesis (MIPO) as an alternative to the conventional open reduction and internal fixation (ORIF) for treating pilon fractures, offering insights into its functional and radiological outcomes, as well as the benefits and limitations of its use.
The following article will dig into existing evidence, highlight the hidden complexities of pilon fracture management, and compare outcomes based on fracture subtypes. Our goal is to provide a thorough perspective to help stakeholders figure a path toward treatment strategies that balance biomechanical stability with soft tissue preservation.
Tricky Parts of Pilon Fracture Management
The distal tibia’s anatomy is packed with small details that make pilon fractures one of the most complicated pieces in trauma care. Pilon fractures stem largely from high-energy trauma – such as falls from height or motor vehicle accidents – and come with considerable soft tissue damage. The treating team must sort out several tangled issues:
- Maintaining Articular Congruity: Rebuilding the smooth surface of the joint is super important to prevent future joint problems.
- Protecting Soft Tissues: The surrounding tissues are easily compromised in high-impact injuries and need careful handling to avoid additional complications.
- Restoring Mechanical Stability: Ensuring the fracture heals correctly requires techniques that provide the necessary support yet do not unduly stress the soft tissue envelope.
The standard ORIF approach offers the advantage of direct visualization of the fracture and the possibility of achieving precise reduction. However, it often involves extensive surgical dissection. This makes the procedure off-putting when it comes to preserving the blood supply and further complicating the soft tissue situation. Given these nerve-racking restrictions of traditional treatment, clinicians are increasingly exploring less invasive options.
Minimally Invasive Plate Osteosynthesis: A Game Changer?
MIPO has emerged as a promising alternative that aims to settle the confusing bits of pilon fracture management. Using smaller incisions, this method minimizes the disturbance to surrounding soft tissues by applying submuscular plate insertion and indirect reduction techniques. Here are some of the key advantages of the minimally invasive approach:
- Soft Tissue Preservation: By avoiding large surgical exposures, MIPO helps maintain the important periosteal blood supply.
- Reduced Risk of Complications: Lowered incidence of wound infections, dehiscence, and necrosis is one of the super important benefits compared to ORIF.
- Biomechanical Stability: Despite being less invasive, MIPO delivers sufficient fracture support essential for union.
These benefits suggest that MIPO may be a preferable choice, particularly in cases where the soft tissues are already loaded with issues due to high-energy impacts. However, any evaluation must weigh these positive aspects against the challenges of accurately aligning the joint surface and ensuring reliable healing over time.
Functional Outcomes: Restoring Mobility and Reducing Pain
The primary aim of any fracture treatment is functional recovery – getting patients back to their everyday lives with minimal pain and restored mobility. Studies assessing MIPO for pilon fractures have noted encouraging improvements in functional outcomes. Metrics such as the American Orthopaedic Foot & Ankle Society (AOFAS) Hindfoot Score and the Olerud and Molander Ankle Score (OMAS) are frequently used to gauge this progress.
One retrospective study involving 33 patients revealed that the mean AOFAS score after one year was 85.2, while the OMAS score averaged 78.4. These numbers indicate a transition from the preoperative state – where pain and dysfunction were high – to a level where most patients reported excellent or good functional recovery. Moreover, the visual analog scale (VAS) for pain saw a dramatic drop from an average of 7.8 before surgery to just 1.5 at one year postoperatively.
Such functional improvements are likely attributable to MIPO’s design to protect the soft tissue while delivering stable fixation. By preserving the delicate balance of life-giving blood supply, MIPO allows for early mobilization and decreases the long-term issues related to stiffness and joint degeneration.
Radiological Healing: Tracking Bone Union Over Time
Radiological healing is one of the key areas where MIPO seems to shine. The modified Radiographic Union Scale for Tibial fractures (mRUST) is a tool used to peek into the healing progress at various intervals following the surgery. In the study mentioned earlier, patients demonstrated progressive improvements in mRUST scores:
| Time Point | mRUST Score (Mean ± SD) | Union Rate |
|---|---|---|
| 6 Weeks | 7.2 ± 1.5 | 12.1% |
| 12 Weeks | 10.8 ± 1.3 | 72.7% |
| 24 Weeks | 12.0 ± 0.0 | 93.9% |
This table clearly shows the fine points of radiological healing – early progress is promising, with nearly full union reported by 24 weeks. Such results compare favorably to traditional methods such as ORIF, where extensive soft tissue dissection can sometimes delay bone healing due to disturbance in blood flow and tissue trauma.
Comparative Outcomes: AO/OTA 43-B vs. 43-C Fractures
Not all pilon fractures are created equal. The AO/OTA classification distinguishes them into types 43-B and 43-C, with 43-C fractures typically involving more comminution and fragmented bone. Studies examining the outcomes of MIPO have revealed some interesting differences between these subtypes:
- Functional Recovery: Patients with the less complicated AO/OTA 43-B fractures reported a higher mean AOFAS score (88.3) compared to the more tangled issues seen in 43-C fractures (mean AOFAS score of 81.5). This difference suggests that the simpler fracture types might benefit more from the functional preservation that MIPO provides.
- Healing Time: In line with functional scores, 43-B fractures tended to heal faster, averaging union at around 18.1 weeks, while 43-C fractures required roughly 22.4 weeks. The delay in the more severe fracture pattern is understandable given the additional nerve-wracking challenges in aligning more fragmented bone fragments.
- Complication Rates: Although the complication rate was slightly higher in 43-C fractures (13.3%) compared to 43-B fractures (5.6%), this difference did not reach statistical significance in the examined cohort. This suggests that while the risk of complications may be slightly increased in more severe injuries, the overall effectiveness of MIPO remains encouraging.
These data points serve as a reminder that while MIPO offers undeniable advantages, patient selection and fracture characteristics remain key to optimizing outcomes. Future studies with larger groups could help clarify these differences further.
Assessing Postoperative Complications
One of the most compelling arguments in favor of MIPO lies in its reduced postoperative complication profile. Traditional ORIF is notorious for its high rates of wound complications, which can include infections, tissue dehiscence, and even necrosis. In contrast, MIPO exhibits a much lower rate of issues, which can be appreciated by looking at the reported outcomes:
| Complication | Incidence |
|---|---|
| Superficial Infection | 6.1% (2 out of 33 patients) |
| Delayed Union | 3.0% (1 out of 33 patients) |
| Nonunion / Implant Failure | 0% |
The above table underscores a critical benefit of minimally invasive techniques: by reducing the extent of surgical exposure, the risk of wound complications is minimized. For many patients and their families, this translates to a smoother recovery process and alleviates a number of the nerve-wracking concerns that accompany major surgery.
Long-term Efficacy and the Need for Further Research
While the short-term outcomes favor the use of MIPO for pilon fractures, questions remain about its long-term efficacy. A follow-up period of 12 months, while useful for assessing union rates and initial functional recovery, may not capture the full spectrum of post-traumatic complications such as arthritis and chronic pain. In the world of orthopaedics, patient-wide robust data are essential for drawing definitive conclusions about the durability of a technique.
Some key areas that future studies should aim to address include:
- Long-Term Joint Health: Monitoring for signs of post-traumatic arthritis is critical, as even a well-healed fracture can lead to subtle joint degeneration over time.
- Patient Satisfaction Over Time: While initial improvements in functional scores are promising, patient satisfaction in the long run is influenced by a variety of factors, including pain management and mobility in everyday activities.
- Comparative Studies: Balanced, prospective research comparing MIPO with ORIF and other contemporary methods will help solidify MIPO’s role in the treatment algorithm.
Addressing these points in multicenter studies with larger cohorts is super important. Only with an expanded evidence base can clinicians confidently recommend MIPO across a wider array of clinical scenarios.
Practical Considerations for Clinicians
For surgeons and healthcare professionals, the decision to use MIPO over traditional methods is not one to be made lightly. The technique demands advanced imaging support, typically fluoroscopy, and expertise in handling indirect reduction strategies through small incisions. As such, certain practical points should be kept in mind when considering MIPO:
- Patient-specific Factors: Age, overall health, bone quality, and the extent of soft tissue damage should all be factored into the decision-making process.
- Surgical Expertise: MIPO is a technique that has a learning curve. The success of the procedure heavily relies on the surgeon’s ability to steer through the subtle details of the fracture without compromising on alignment.
- Facility Resources: Having access to high-quality imaging and specialized operating room equipment is key to making the technique work effectively.
Clinicians must therefore weigh the potential benefits of reduced soft tissue trauma against the technical challenges, ensuring that each patient’s unique scenario is carefully considered. Tailoring the approach to individual needs remains a key part of finding the best path forward in fracture management.
Economic and Societal Impacts
The use of minimally invasive techniques like MIPO also carries implications that extend beyond the operating room. Shorter hospital stays, lower complication rates, and a quicker return to normal activities not only benefit patients but also help reduce overall healthcare costs. In environments where healthcare resources are stretched thin, employing methods that minimize postoperative issues can be the difference between a smooth recovery and a prolonged, expensive treatment timeline.
From a societal perspective, quicker recoveries mean less time off work, reducing the economic impact on both families and employers. Additionally, fewer complications translate to fewer readmissions and follow-up procedures – a super important point in managing healthcare budgets and ensuring efficient use of resources.
These economic benefits, while hard to quantify in every case, add another layer to the argument in favor of adopting MIPO techniques for pilon fractures, especially in high-volume trauma centers.
Critical Analysis: Weighing the Pros and Cons
No single surgical technique is without its limitations. While MIPO shows clear benefits in terms of soft tissue preservation and lower complication rates, it is not free from challenges. Here are some of the potential downsides that clinicians must take into account:
- Learning Curve: The technique requires precision through small incisions, which means that surgeons must be well-trained and experienced. In inexperienced hands, the outcomes might not match the promising results noted in specialized centers.
- Limited Direct Visualization: Unlike ORIF, where the fracture site is fully exposed, MIPO relies on indirect reduction methods. This can sometimes lead to less-than-perfect alignment of the articular surface, particularly in more complicated cases.
- Equipment Demands: The reliance on high-quality imaging technology such as fluoroscopy mandates an infrastructure that may not be universally available, especially in resource-constrained settings.
It is also important to realize that while complication rates appear lower with MIPO, there is always a need for careful patient follow-up. Subtle issues such as malalignment can sometimes be missed in the short run and only become apparent over longer periods. In this light, ongoing monitoring and larger, randomized studies are necessary to truly delineate the benefits and pitfalls of MIPO relative to traditional techniques.
Patient Perspectives and Shared Decision-Making
When considering any surgical intervention, it is crucial to not only focus on clinical outcomes but also include patient preferences. From the perspective of many affected by pilon fractures, the avoidance of large incisions and the possibility of quicker recovery times are very appealing. Patients often report a greater sense of satisfaction when they experience less postoperative discomfort and quicker functional return.
Shared decision-making – where the surgeon and patient work together to choose the best treatment path – requires that the patient be adequately informed about the subtle details and potential risks associated with both MIPO and ORIF. Some of the factors that patients might weigh include:
- Recovery Time: Faster bone healing and reduced pain can be significant drivers in favor of minimally invasive techniques.
- Cosmetic Outcome: Smaller incisions typically result in less scarring, which can be important for many patients.
- Long-Term Functionality: Ensuring that the joint functions well in the long run is critical, particularly for active individuals.
This approach to healthcare is key to ensuring that the patient’s individual priorities are respected, making it a must-have component of modern trauma care.
Long-Term Implications for Orthopaedic Practice
If we take a step back to evaluate the broad implications of adopting MIPO for pilon fractures, several trends become apparent. First and foremost, there is a growing body of evidence that supports the role of minimally invasive techniques in reducing overall morbidity. As more surgeons get trained in these methods, we can expect a gradual shift in the standard of care, particularly for cases of high-energy trauma where soft tissue preservation is critical.
In addition, incorporating MIPO into clinical practice has the potential to foster a more refined approach to fracture management. By embracing a method that minimizes surgical trauma, the orthopaedic community may be able to reduce the incidence of long-term complications that have historically plagued patients treated with open procedures.
There is also a call within the community for further research to ascertain the fine shades of clinical outcomes based on patient demographics and fracture patterns. Such research could lead to more in-depth guidelines and help determine the optimal criteria for selecting patients for MIPO. Ultimately, this could ensure that the right treatment is matched with the right patient, maximizing benefits and minimizing risks.
Future Directions and Research Needs
While MIPO presents many advantages in managing pilon fractures, the current data points must be expanded to include long-term outcomes, larger sample sizes, and randomized controlled trials. Future research topics worth exploring include:
- Extended Follow-Up Studies: Tracking patients beyond the one-year mark to evaluate the emergence of degenerative changes in the joint or late complications such as chronic pain and arthritis.
- Comparative Studies: Direct comparisons between MIPO and ORIF can yield insights into which technique best balances early functional recovery with long-term joint preservation.
- Cost-effectiveness Analyses: Given the potential economic benefits of quicker recoveries and lower complication rates, analyses in this area can help hospitals and payers make more informed decisions.
- Patient-centered Outcomes: Expanding outcome measures to include quality of life assessments and patient satisfaction scores will help capture the full impact of these surgical methods.
By addressing these research gaps, the orthopaedic community can further validate the role of MIPO and continue to refine surgical techniques to better serve patients with pilon fractures.
Summary of Key Findings and Takeaways
To summarize, minimally invasive plate osteosynthesis (MIPO) offers a promising alternative for the treatment of pilon fractures by addressing some of the tricky parts and hidden complexities inherent in these injuries. The following bullet points capture the essence of our findings:
- MIPO leverages small incisions and indirect reduction methods to preserve the soft tissue envelope, which is critical to ensuring a smooth healing process.
- Functional outcome measures, such as the AOFAS and OMAS scores, show significant improvement one year post-surgery, with a marked decrease in associated pain levels.
- Radiological assessments using the mRUST score reveal a steady progression toward bone union, with nearly 94% of patients achieving full union by 24 weeks.
- Comparative studies indicate that patients with AO/OTA 43-B fractures tend to experience faster healing and better functional recovery compared to those with 43-C fractures; however, the limited sample size necessitates further research.
- The overall complication rate associated with MIPO is low, particularly when compared to traditional ORIF methods, making it a super important option for cases with compromised soft tissues.
- Further research should focus on long-term outcomes, cost-effectiveness, and patient-centered measures to refine treatment protocols and ensure the technique’s reliability over time.
Concluding Thoughts: Balancing Innovation with Caution
In the ever-evolving field of orthopaedic trauma, innovations like minimally invasive plate osteosynthesis represent a significant step forward. MIPO addresses many of the challenges – from the confusing bits of fracture reduction to the delicate preservation of surrounding soft tissues – that have traditionally made pilon fractures a nerve-wracking area for surgeons.
While current evidence is encouraging, it is important to note that the available studies are often limited by relatively small sample sizes and short follow-up durations. As such, while many clinicians are enthusiastic about the benefits of MIPO, a careful and measured approach remains necessary. Surgeons and healthcare decision-makers should consider individual patient characteristics, infrastructure availability, and long-term data when choosing the most appropriate treatment strategy.
The discussion surrounding pilon fracture management is far from settled. It is clear that both the functional recovery of patients and the integrity of radiological healing are crucial elements in determining the best course of action. With the right combination of innovation and careful patient management, MIPO could very well form the backbone of future standards in the treatment of these intimidating injuries.
Looking Ahead: The Road to Enhanced Patient Outcomes
As more centers adopt MIPO as a preferred method for managing pilon fractures, we can expect a paradigm shift in treatment practices. The results seen thus far pave the way for more expansive studies and a gradual rethinking of traditional approaches. Key future directions include:
- Multicenter Studies: Bringing together data from various institutions will help overcome the limitations of small cohorts and provide a more robust statistical basis for evaluating MIPO’s effectiveness.
- Standardizing Protocols: Establishing uniform guidelines on patient selection, surgical timing, and postoperative care can help doctors find their way through the subtle differences and ensure a consistent high standard of care.
- Enhanced Training Programs: Focused training initiatives and surgical workshops on minimally invasive techniques will equip new surgeons with the skills necessary to manage these tricky fractures safely and effectively.
- Patient Follow-up Regimens: Long-term follow-up will be essential to fully understand the impact of MIPO on joint health and overall quality of life, thereby addressing the lingering questions about the durability of the results.
By continuing to invest in these areas, the field of orthopaedic trauma can work toward ensuring that patients not only experience faster recoveries but also enjoy sustained joint function and overall well-being long after the initial treatment.
Final Reflections
The journey to improving outcomes in pilon fracture management is layered with both promising innovations and challenging twists and turns. MIPO offers a balanced approach to achieve both the biomechanical stability needed for bone healing and the essential soft tissue preservation that promotes rapid recovery and reduces the likelihood of serious complications.
While the current data presents a reassuring picture, comprehensive research and long-term follow-up remain critical. Balancing innovation with prudence, the medical community must continue to dig into the available data while also embracing new techniques that could revolutionize patient care.
In this delicate game of balancing the hidden complexities of pilon fractures, every small twist and every subtle detail matters. Whether it’s the shorter recovery times, improved cosmetic outcomes, or lower risk of infection, the minimally invasive approach is gradually carving out its niche in orthopaedic trauma care.
For patients facing the reality of a pilon fracture, the choice between conventional open surgery and a minimally invasive option is fraught with implications for both short-term recovery and long-term joint health. It is our view that the evidence increasingly supports giving patients access to MIPO, especially in cases where soft tissue safety is paramount. However, individual circumstances and sound clinical judgment must always guide treatment decisions.
Ultimately, as the field continues to evolve, the focus must remain on delivering care that is both effective and compassionate, ensuring that each patient’s unique needs are met with the very best that modern medicine has to offer. With continued advances in surgical technology and technique, we are optimistic about a future where even the most intimidating injuries can be managed with confidence and a high degree of success.
This opinion editorial serves as a reminder that while challenges remain, the current trajectory of research and clinical practice promises a brighter horizon. Minimally invasive techniques like MIPO are not just about reducing recovery times – they are about transforming lives and redefining the treatment landscape for pilon fractures. As we step into this new era, the commitment to innovation, patient safety, and continuous learning will guide us forward.
Originally Post From https://www.cureus.com/articles/401422-determining-the-outcomes-of-pilon-fractures-treated-by-minimally-invasive-plate-osteosynthesis-mipo-a-retrospective-study
Read more about this topic at
Effectiveness of Minimally Invasive Plate Osteosynthesis …
Determining the Outcomes of Pilon Fractures Treated by …