Modern Approaches in Gastric Cancer Treatment: A Closer Look at ESD
Recent research published in BMC Cancer has sparked considerable conversation among healthcare professionals by suggesting that endoscopic submucosal dissection (ESD) is a safe, minimally invasive alternative to traditional surgery for early gastric cancer (EGC) in patients under the age of 45. In this editorial, we will take a closer look at the study’s findings, the pros and cons of ESD, and its potential impact on treatment strategies in modern medicine. We will also explore alternative perspectives around modern treatment trends and discuss the practical implications for younger patients facing the challenges of EGC.
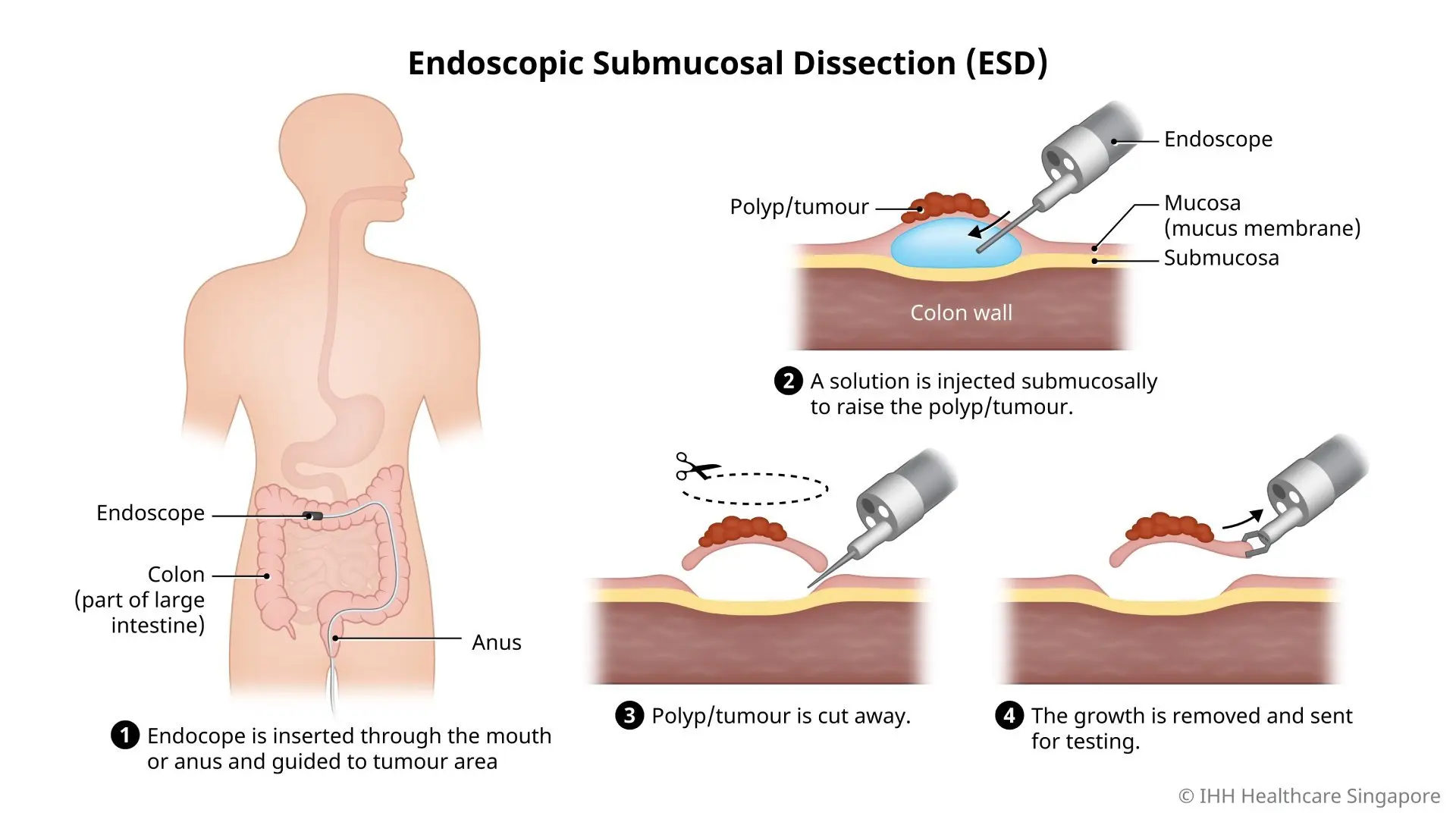
Understanding Endoscopic Submucosal Dissection
ESD is a technique that removes cancerous lesions from the stomach lining by lifting and cutting the lesion away with specialized tools. This method is less invasive compared to conventional surgical resection, aiming to reduce recovery times and complications. The study in question evaluated survival rates, recovery patterns, and the risk of complications when comparing ESD with standard surgery.
Key Features of ESD
- Minimally Invasive – ESD is performed using an endoscope, reducing the need for large incisions.
- Precision Removal – The technique focuses on excising only the affected tissue, preserving more of the healthy stomach.
- Rapid Recovery – Patients may experience a shorter hospital stay with less post-procedure discomfort.
- Comparable Outcomes – Evidence suggests that survival rates for ESD are on par with those for traditional surgical methods.
Young Patients and Early Gastric Cancer: A Special Consideration
The study particularly focused on patients younger than 45, a demographic that typically presents with unique challenges and health concerns. The less invasive nature of ESD can be particularly appealing for this group, as younger individuals often value faster recovery times and fewer disruptions to their personal and professional lives.
Why Early Gastric Cancer in the Young Is Different
Younger patients with EGC are not only dealing with the emotional shock of a cancer diagnosis but also the added pressure of maintaining an active lifestyle during their recovery. The advantages of ESD include:
- Less Post-Operative Pain – The reduced trauma of the procedure means less pain and discomfort.
- Shorter Hospital Stays – Recovering at home can be less intimidating and allows for a return to normal life sooner.
- Preserved Organ Function – With more of the stomach preserved, nutritional absorption and digestion might remain largely undisturbed.
This treatment modality is especially important when the tricky parts of a traditional surgery—such as extensive incisions and a longer recovery trajectory—are taken into account. Younger patients can greatly benefit from a procedure that offers fewer tangled issues and complications along the way.
The Safety and Efficacy Debate: ESD Versus Traditional Surgery
One of the cornerstones of modern cancer care is the delicate balance between intervention effectiveness and patient quality of life. ESD is now entering the conversation as a possible substitute for conventional surgery when managing early gastric cancer. Analyzing survival outcomes, complication rates, and patient recovery data provides a thorough picture of this emerging treatment option.
Comparing Survival Rates and Recovery Outcomes
The study found that the survival rates for patients undergoing ESD are very similar to those who opt for traditional surgery. The minimal invasiveness of ESD, however, gives it an edge when it comes to recovery profiles. Here is a simplified table to illustrate some of the key differences:
| Parameter | ESD | Conventional Surgery |
|---|---|---|
| Invasiveness | Minimally invasive – less bodily trauma | Highly invasive – significant incisions required |
| Hospital Stay | Shorter duration | Longer, sometimes nerve-racking recovery period |
| Recovery Time | Faster return to daily life | Prolonged recovery, often with complications |
| Complication Risk | Lower risk for post-procedure complications | Higher risk of infections and other issues |
Having a consolidated overview like this is super important, as it gives both patients and clinicians a clear understanding of the finer shades in each treatment option.
Examining the Longer Term Implications of Minimally Invasive Techniques
While the study supports ESD as an effective treatment option for young EGC patients, it also calls for a broader evaluation of how minimally invasive techniques could reshape gastric cancer management in the coming years. The shifts in treatment style offer several key benefits and challenges that warrant discussion, especially when we consider the complicated pieces of modern medical therapy.
Key Benefits of Minimally Invasive Methods
When managing a condition like early gastric cancer, the less invasive a treatment is, the better the quality of life might be for the patient. Some of these benefits include:
- Preservation of Normal Anatomy: The importance of maintaining normal stomach structure cannot be overstated. Less tissue removal means better functional outcomes.
- Reduced Stress on the Body: A treatment that avoids large incisions significantly reduces the overall physical burden on a patient’s system.
- Fewer Complications: With fewer twisted procedures and reduced trauma, the risk of complications like infections or excessive bleeding is greatly minimized.
- Quicker Return to Routine: For the young and active, being able to swiftly return to work and family life is key. ESD offers that possibility by reducing downtime.
Practitioner Perspectives on Treatment Options
Doctors often have to weigh the benefits against the potential risks inherent in any procedure. With ESD, while the technique seems promising, it is not completely without its own set of challenges. For instance:
- Technical Demands: The procedure requires a high level of skill and precision from the endoscopist. This means that only practitioners with specialized training should perform it.
- Risk of Incomplete Resection: In some cases, if the dissection is not executed perfectly, there might be residual cancerous tissue that requires additional intervention.
- Patient Selection: Not every patient is an ideal candidate for ESD. Determining who will benefit most from this technique is critical and requires a detailed pre-procedure evaluation.
These points illustrate that while ESD could be a key treatment method, making your way through the decision-making process is a task full of problems that must be addressed carefully. The subtle parts of the planning and execution are essential to ensure the patient receives the best possible outcome.
Critical Factors to Consider When Choosing a Treatment Strategy
Deciding between ESD and conventional surgery can be intimidating for both patients and physicians. To facilitate a more informed decision, several key factors need to be integrated into the assessment process. Below is a detailed discussion of these important considerations.
Patient’s Overall Health and Lifestyle
One of the most critical aspects of selecting a treatment method is assessing the patient’s overall health and daily life demands. Young individuals often have fewer comorbid conditions and robust physical resilience, which can influence the choice of a less invasive treatment. Considerations include:
- Activity Level: Active patients may prefer methods that allow for faster mobility and return to sports or work.
- Coexisting Conditions: Even in younger patients, the presence of underlying conditions can complicate surgical recovery.
- Nutritional Status: Since the stomach plays a key role in digestion, preserving its function is super important for maintaining proper nutrition.
Technical Feasibility and Experience
Not all medical centers or practitioners may have the expertise or technology to perform ESD reliably. This creates a situation where choosing a treatment strategy is a bit like trying to figure a path through tricky parts. Factors include:
- Availability of Skilled Endoscopists: Expertise can significantly influence both the success rate of the procedure and the risk profile for complications.
- Technological Resources: Modern endoscopic tools are essential for the delicate dissection required in ESD.
- Institutional Experience: Hospitals and clinics with a history of performing ESD tend to have more refined post-procedure care protocols.
Here is a simple table summarizing these considerations:
| Factor | Implication |
|---|---|
| Patient’s Health & Lifestyle | Determines tolerance for procedures and speed of recovery |
| Technical Expertise | Directly impacts the success and safety of ESD |
| Institutional Experience | Ensures robust follow-up and management of complications |
Managing Expectations and Addressing Concerns
For many patients, navigating through the decision between modern, less invasive techniques and traditional surgery can seem overwhelming. The information sometimes comes in a mix of straightforward facts and confusing bits of medical jargon. It becomes essential to manage expectations and reassure patients while addressing their fears in a clear and friendly manner.
Communication Is Key
It is super important for healthcare providers to:
- Simplify Medical Jargon: Explaining the procedure in simple terms helps demystify the process.
- Discuss Potential Outcomes: Honest discussion about both the benefits and the risks of each treatment option is necessary.
- Provide Visual Aids: Diagrams and procedure flowcharts can help patients understand how ESD works compared to conventional surgery.
Doctors should stress that the aim of any treatment is not just to remove the cancer but also to ensure that the patient can quickly resume a normal, healthy lifestyle without being burdened with long-term complications. Such clarity helps reduce the nerve-racking nature of facing a new diagnosis or a major procedure.
Alternative Perspectives from the World of Modern Medicine
While the evidence for ESD is growing, it is critical to understand that medicine is full of twists and turns. Different perspectives exist, especially as we compare modern techniques with more established surgical methods. In this context, it is useful to consider views from both proponents and skeptics of the minimally invasive approach.
Proponents of ESD
Advocates for the widespread adoption of ESD highlight several benefits that include:
- Less Bodily Trauma: The argument is that reducing the physical impact of the procedure can lead to better overall patient outcomes.
- Enhanced Quality of Life: With faster recovery times and fewer complications, patients can return to their daily routines with minimal interruption.
- Cost-Effectiveness: Shorter hospital stays and fewer post-operative complications may reduce overall treatment costs.
Skeptics and Their Concerns
On the other hand, some experts remain cautious. Their concerns often center around:
- Limited Data in Diverse Populations: While promising, many studies on ESD have small sample sizes or are limited to specific regions or institutions.
- Technical Challenges: The success of the procedure heavily depends on the practitioner’s expertise. Inexperience can lead to incomplete resections and potential recurrences.
- Long-Term Outcomes: Critics emphasize the need for long-term follow-up data to definitively assess the risk of cancer recurrence and overall survival.
These contrasting opinions remind us that every treatment option comes with its own set of little twists. It is crucial, therefore, for both doctors and patients to digest all available information before making a decision.
Integrating Alternative Medicine Perspectives
While modern minimally invasive procedures like ESD dominate the conversation in gastric cancer treatment, there is also growing interest in complementary approaches. Many patients and practitioners are increasingly open to integrating alternative medicine perspectives with established treatments to support holistic healing.
Complementary Approaches for a Holistic Recovery
Alternative therapies can play a role—especially when it comes to easing the recovery process following a medical procedure. Some strategies include:
- Nutritional Support: Tailored diets, rich in vitamins and minerals, help strengthen the body while it heals. Super important foods and supplements can be recommended by nutritionists with a focus on rebalancing the body’s internal machinery.
- Mind-Body Practices: Meditation, yoga, and other relaxation techniques can help manage stress and improve overall well-being. These activities serve as a calming counterbalance to the sometimes intimidating aspects of cancer treatment.
- Herbal Supplements: Some herbal remedies may offer anti-inflammatory or immune-boosting benefits. However, caution should be taken, and these should be discussed with a doctor before incorporation into the treatment plan.
Integrative Medicine: Finding Your Path Through Combined Practices
Integrative medicine takes a balanced approach by combining modern treatments with holistic practices. This method does not replace the need for proficient medical intervention but offers support in managing the fine points of overall health and recovery. Here are some key benefits:
- Personalized Treatment: Tailoring recovery plans that combine the best of modern medical procedures with alternative therapies can lead to improved outcomes.
- Emotional Well-Being: Addressing both physical and emotional health needs can reduce the overwhelming stress associated with cancer diagnosis and treatment.
- Enhanced Immune Function: With the proper support, patients may experience better immune function during the healing process.
It is essential to remember that while integrative approaches offer potential benefits, the primary treatment should be based on solid clinical evidence and performed by skilled professionals. Working through the combined strategies can be challenging but ultimately rewarding for overall patient care.
Addressing the Tricky Parts of Clinical Decision Making
Together, the evidence and opinions on ESD underline the fact that clinical decisions, especially those involving cancer treatment, are riddled with complicated pieces and subtle details. Both patients and clinicians must work closely to assess options while keeping personal health goals in mind. The conversation often revolves around:
Key Factors in Decision Making
- Risk vs. Reward: Weighing the benefits of a minimally invasive procedure against the potential for technical issues or incomplete resection.
- Experience and Expertise: Considering whether the available healthcare team has the necessary know-how to perform ESD effectively.
- Patient Preferences: Incorporating the voice and values of the patient into the treatment plan helps ensure that decisions align with the individual’s lifestyle and expectations.
To better organize these factors, consider the following checklist that might help in making a well-informed choice:
- Have you discussed all potential advantages and concerns with your healthcare provider?
- Do you have access to a team experienced in performing ESD?
- Have you considered both modern techniques and supportive alternative treatments?
- Are your expectations in line with the overall recovery timeline and possible complications?
This checklist provides a practical tool for patients facing the sometimes intimidating process of clinical decision making. It can serve as a starting point for discussions and help both parties figure a path through the tricky parts of the treatment landscape.
Future Trends in Gastric Cancer Treatment and Research
As research continues to expand our understanding of cancer therapies, it is clear that innovative techniques like ESD will play an increasingly prominent role in treatment plans. The findings discussed here represent not just a snapshot of current trends, but a glimpse into the future of targeted, minimally invasive care in oncology.
Emerging Technologies and Their Impact
Researchers around the world are exploring new tools and methods that build upon current techniques. Some exciting future directions include:
- Robotic Assistance: Integrating robotics into ESD procedures could help reduce the small twists and unpredictable bits of human error, resulting in even more precise interventions.
- Advanced Imaging: Improved imaging techniques may allow doctors to get into even finer details of the cancerous tissue, ensuring complete and effective resection.
- Personalized Medicine: As genetic and molecular profiling improves, treatments may be increasingly tailored to individual patient characteristics, ensuring better outcomes while managing complicated pieces of the overall treatment puzzle.
These innovations are expected to not only augment the safety and effectiveness of procedures like ESD but also contribute to a broader shift in how gastric cancer is managed. With each advancement, practitioners and patients alike will have more resources to steer through the challenges of cancer treatment.
Ongoing Research and Collaborative Efforts
Ongoing clinical trials and collaborative research efforts are critical to validating the potential of ESD on a larger scale. Here are some key areas of focus that researchers are currently exploring:
- Long-Term Survival Data: While short-term outcomes are promising, gathering long-term data is essential for confirming the durability of ESD’s benefits.
- Quality of Life Assessments: Comparative studies that evaluate not just survival rates, but overall quality of life, mental health, and post-procedure satisfaction.
- Cost-Benefit Analysis: Determining the economic viability of widespread ESD implementation in various healthcare systems.
- Technical Standardization: Establishing standardized protocols and training programs can help minimize the fine points of variation between practitioners.
This comprehensive approach to evaluating new treatment methods ensures that every little twist and nuanced detail is taken into account, ultimately enhancing the standard of care for patients facing early gastric cancer.
Conclusion: A Balanced Perspective on ESD and Conventional Surgery
Endoscopic submucosal dissection has emerged as a promising alternative to conventional surgery for young patients with early gastric cancer. Its minimally invasive nature, fast recovery time, and comparable survival outcomes offer a compelling treatment option for a demographic that is both active and eager for recovery with minimal interruptions.
However, it is important to recognize that every treatment method comes with its own set of challenging parts. Issues such as practitioner expertise, technical feasibility, and long-term outcomes must all be considered carefully. As we continue to poke around in this evolving landscape, both modern medicine and integrative approaches can work in tandem to provide the best possible care for patients.
Ultimately, the choice between ESD and traditional surgery should be made on a case-by-case basis, with thorough consultation between the patient and the clinical team. By managing their way through the detailed, sometimes tangled issues of diagnosis and treatment, patients can achieve a balanced and well-informed decision that aligns with their values and lifestyle goals.
The road ahead is full of promising innovations and collaborative research. As we figure a path through the twists and turns of gastric cancer treatment, adopting a personalized and holistic approach will be critical in ensuring that every patient receives care that is both effective and empathetic.
In summary, the findings from the study present a hopeful alternative amid the challenging landscape of oncology care. With continued research and technological advancements, minimally invasive techniques like ESD could soon become a standard first-line treatment for young patients with early gastric cancer, marking a significant milestone in the evolution of modern cancer therapy.
Originally Post From https://www.geneonline.com/study-finds-endoscopic-submucosal-dissection-as-a-safe-alternative-to-surgery-for-early-gastric-cancer-in-patients-under-45/
Read more about this topic at
Minimally invasive surgery
What Alternatives Has Minimally Invasive Surgery Provided …