Systemic Inflammation in HIV: An Opinion on the Switch from Dual to Triple ART Regimens
The management of HIV is full of tricky parts, especially when it comes to finding the right balance between effective viral suppression and mitigating long-term complications. A recent phase IV trial—known as the INSTINCT/GESIDA10918 study—provides thought-provoking insights into whether switching from a dual antiretroviral therapy (ART) regimen to a triple regimen modifies systemic inflammation or metabolic outcomes. In this editorial, we take a closer look at the study’s results, review the fine points of inflammatory and metabolic changes, and offer some reflections on how clinicians can get around these challenges in everyday practice.
At its essence, the study evaluated adults with HIV-1 infection who had achieved viral suppression on a dolutegravir plus lamivudine (DTG/3TC) regimen. The objective was to test if moving to a regimen consisting of bictegravir, emtricitabine, and tenofovir alafenamide (BIC/FTC/TAF) might improve inflammatory markers over 96 weeks. With over 140 participants enrolled from 19 Spanish hospitals, the trial presents a unique opportunity to poke around the subtle parts of ART regimen effectiveness in terms of inflammation and metabolic health.
Examining the Study Design: The Backbone of the Analysis
The INSTINCT/GESIDA10918 study was set up as a prospective, open-label, multicenter, randomized clinical trial. Its primary goal was to assess whether a switch from a dual regimen (DTG/3TC) to a triple regimen (BIC/FTC/TAF) leads to meaningful changes in a set of systemic inflammation biomarkers. The trial design was careful and straightforward: adults who had maintained plasma HIV-1 RNA levels below 50 copies/mL for at least 48 weeks on DTG/3TC were randomly assigned either to continue their dual therapy or to switch regimens.
The detailed approach included:
- Full consideration of patient demographics and clinical history, ensuring that both treatment groups were balanced.
- A follow-up period, stretching over 96 weeks, for a thorough look at clinical and laboratory outcomes.
- A focus on a range of inflammatory biomarkers as well as metabolic and renal parameters.
This methodical approach helps both experts and clinicians figure a path in interpreting the efficacy and safety of treatment adjustments in controlled HIV. It also provides insight into the nitty-gritty of how subtle shifts in medication combinations might—or might not—translate into clinical benefits.
Understanding the Tricky Parts of ART Switching
Switching ART regimens is never as simple as it might seem at first glance. Despite the promise of newer drug combinations, there are tangled issues that can emerge when altering treatment, even when the patient is already enjoying a well-suppressed viral load. The trial investigators hoped that moving to a triple regimen might offer additional metabolic or inflammatory benefits, but the findings suggest otherwise.
Some of the challenging aspects include:
- Systemic Inflammation: Inflammatory biomarkers such as interleukin-6 (IL-6), sCD14, sCD163, high-sensitivity C-reactive protein (hsCRP), D-dimer, and the kynurenine/tryptophan (K/T) ratio were measured to evaluate any potential benefit from switching ART. These markers are considered key in understanding inflammation-driven comorbidities.
- Metabolic Parameters: Changes in weight, lipid profiles, and renal function were also closely monitored. Even minor advancements in these components could indicate a better strategy for managing the chronic issues associated with HIV therapy.
- Long-Term Outcomes: While the short-term efficacy of dual versus triple regimens may appear equivalent in maintaining viral suppression, the long-term clinical implications, particularly those related to inflammation, remain intimidating in their full scope.
Even with high-level viral suppression in both groups, the study found that changes in inflammatory and metabolic markers were minute, demonstrating that modern ART regimens might have limited impact on the residual inflammation associated with HIV. This mirrors many real-world clinical scenarios where the switch between approved regimens does not always translate to significant clinical improvement in systemic inflammation.
Diving into the Systemic Inflammation Findings
One of the most intriguing aspects of the trial is its focus on inflammatory biomarkers. These biomarkers reveal the hidden complexities of how HIV and its treatments interact with the body’s immune system. Clinicians have long sought alternative interventions to specifically target inflammation-driven comorbidities, and the current study sheds light on why this remains a work in progress.
The main inflammatory markers assessed were:
- Interleukin-6 (IL-6): A cytokine involved in the immune response. Elevated levels have been linked with increased cardiovascular risks.
- sCD14 and sCD163: These soluble markers are indicators of monocyte/macrophage activation, offering clues into the state of systemic inflammation.
- High-Sensitivity C-Reactive Protein (hsCRP): A well-known marker used in assessing cardiac risk and overall inflammatory status.
- D-dimer: A protein fragment observed following blood clot breakdown, elevated levels of which may signal vascular complications.
- Kynurenine/Tryptophan Ratio: A marker that indirectly reflects immune activation and inflammation.
Importantly, the study recorded no significant differences between the dual and triple regimens over the 96-week period for any of these markers. This outcome is best understood when we consider that once viral suppression is well-maintained, the body may already have compensated as much as it can in terms of controlling inflammation. That said, it also suggests that simply changing ART regimens may not be enough; clinicians may need to consider supplementary strategies to address these confusing bits.
Metabolic Outcomes and Weight Changes: Looking at the Fine Points
In parallel with the inflammatory analysis, the study also took into account metabolic parameters. These components, although often regarded as secondary outcomes, are super important in evaluating the overall impact of treatment changes on a patient’s health.
Key metabolic outcomes included:
- Body Weight: An interesting observation was that both treatment groups experienced modest weight gains over the study period—with approximately 20% of participants experiencing gains of more than 5%. The slight increases in weight did not differ significantly between the dual and triple therapy groups, which might point to underlying metabolic regulation beyond the scope of the medication regimen.
- Lipid Profiles: Total cholesterol, low-density lipoproteins (LDL), high-density lipoproteins (HDL), and triglycerides showed minimal changes. These lipid parameters are a critical part of the nutritional and cardiovascular assessment in patients undergoing ART.
- Renal Function: Both estimated glomerular filtration rate (eGFR) and serum creatinine levels maintained a steady trajectory, suggesting that switching regimens did not introduce additional challenges with kidney function.
One might have hoped that a more robust treatment regimen could positively affect these metabolic pieces, yet the study reinforces that when viral suppression is maintained, the metabolic benefits of switching are not markedly different. This observation offers a calm reminder that many issues in ART management are loaded with subtle details that require a comprehensive, multifaceted approach.
Reviewing the Safety Profile and Side Effects: A Nitty-Gritty Look
Safety remains one of the most critical components when deciding on any therapy adjustment, including ART switching. The reported adverse events (AEs) from the study were largely mild—categorized as grade 1 or 2—and tended to be self-limited. However, the reports also note that drug-related AEs were slightly more frequent in the group that switched to BIC/FTC/TAF. These included issues such as transient insomnia, fatigue, and gastrointestinal discomfort.
For clarity, the key safety observations include:
| Parameter | DTG/3TC (Dual Therapy) | BIC/FTC/TAF (Triple Therapy) |
|---|---|---|
| Virologic Suppression Rates | >95% | >95% |
| Grade 1-2 Adverse Events | Similar Rates | Similar Rates |
| Drug-Related AEs | 0.4% reported | 4.8% reported, including transient insomnia, fatigue, and GI discomfort |
| Renal Function Changes | Stable | Stable |
This table makes it clear that while both regimens are safe and effective in keeping HIV under control, the triple regimen may bring slightly higher rates of mild, self-limited side effects. For many patients and clinicians, these added issues may seem like small distinctions; however, for those who are sensitive to even minor gastrointestinal or sleep disturbances, it can be another twist and turn in the complex journey of managing HIV.
Implications for Clinical Practice: Finding Your Path in HIV Management
What lessons can everyday clinicians take away from this study? First and foremost, the research underscores that in a setting where HIV is already well-controlled, switching between modern ART regimens may not address the confusing bits of systemic inflammation. In other words, while the promise of a new regimen can be enticing, the actual clinical benefits—in this case related to inflammation and metabolic parameters—appear minimal.
Some practical takeaways include:
- Assessing Patient Needs Holistically: Clinicians need to steer through both clinical data and patient quality-of-life issues when considering regimen changes. This means weighing the slight advantages in drug safety and the possibility of minor improvements in metabolic outcomes against the risk of increased side effects.
- Beyond ART Adjustments: The negligible differences in inflammatory markers call for alternative strategies. In practice, this might involve adding lifestyle modifications such as nutrition adjustments, exercise programs, or even considering complementary medicine approaches to help reduce systemic inflammation.
- Monitoring Long-Term Effects: Since the study duration was 96 weeks, there is still a need to monitor patients over even longer periods for any delayed benefits or complications. The long-term picture is full of tricky parts that require continuous observation, especially when managing comorbidities that develop slowly over time.
This balanced approach empowers clinicians to make well-informed decisions. Instead of expecting a dramatic shift in systemic inflammation as a result of switching ART regimens, healthcare professionals should consider a more comprehensive plan that targets inflammation on multiple fronts.
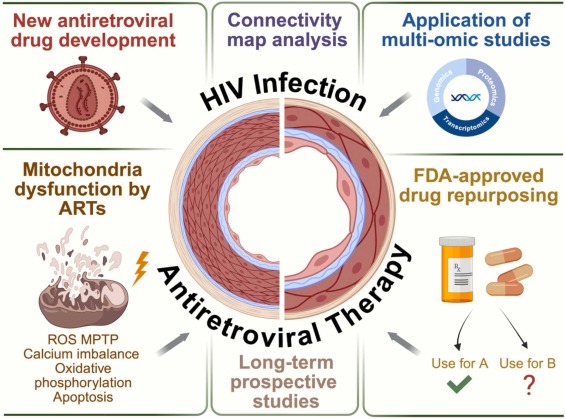
Alternative Strategies for Addressing Inflammation-Driven Comorbidities
If the results from the INSTINCT/GESIDA10918 study indicate that simply altering ART regimens might not be enough, what additional interventions can be considered? The answer likely lies in a multidisciplinary approach that combines medical management with lifestyle interventions.
Some promising strategies involve:
- Anti-Inflammatory Medications: Although standard ART may not significantly impact the inflammatory markers, certain anti-inflammatory drugs could be added to the treatment plan. Research in this area is still full of problems and evolving, but early-phase trials have shown potential benefits in reducing systemic inflammation.
- Nutritional Interventions: Dietary modifications steeped in anti-inflammatory principles (such as diets rich in omega-3 fatty acids, antioxidants, and low in processed sugars) could help manage inflammation. Nutraceuticals and supplements are also being studied for their role in calming the body’s immune responses.
- Exercise Programs: Regular physical activity has been repeatedly shown to lower systemic inflammation. For patients with HIV, integrating moderate exercise regimens can serve as a complementary tool to bolster overall health.
- Stress Reduction Techniques: Psychological stress is known to exacerbate inflammatory responses. Programs incorporating mindfulness, meditation, or even counseling might help alleviate some of the nerve-racking aspects of chronic disease management.
Each of these strategies represents a piece of the puzzle in managing inflammation-driven comorbidities. The key here is that addressing these small distinctions in inflammation requires a multi-pronged approach. Simply switching ART regimens might not suffice when the hidden complexities of chronic inflammation call for interventions that are super important on a holistic level.
Patient-Centered Considerations: The Human Side of ART Adjustments
Equally essential to clinical decisions is the patient’s perspective. ART adjustments, particularly the switch from a dual to a triple regimen, come with a host of personal considerations that go beyond the laboratory values. Patients often face a nerve-racking journey, trying to balance the benefits of viral suppression with the side effects and lifestyle impacts of medications.
Factors influencing the patient experience include:
- Quality of Life: Even if the scientific markers remain stable, patients may experience subjective changes or feel more off-putting side effects with a new regimen. Ensuring that these factors are discussed during consultations is key.
- Psychological Impacts: The process of switching medications can be overwhelming. As patients adjust to new routines and potential side effects, ongoing support from healthcare teams is essential.
- Practical Considerations: Dosing schedules, the number of pills, and even the cost implications can affect adherence. Health professionals must manage your way through these little twists by providing comprehensive education about any planned regimen change.
When patients are fully informed and engaged in the decision-making process, the chances of successful long-term management increase. This patient-centered model not only addresses the visible medical challenges but also helps mitigate the more complex pieces that are part of living with HIV.
Limitations of the Study: The Small Details That Matter
No clinical study is without limitations, and this trial is no exception. The authors acknowledged several factors that may affect how we interpret the results:
- Sample Size: The study enrolled 141 participants, a figure that was somewhat constrained by the challenges of recruitment during the COVID-19 pandemic. A larger cohort might have revealed subtle differences that were not detectable in this analysis.
- Demographic Skew: With the vast majority of participants being male and Caucasian, the findings may not fully extend to other populations, particularly women or racial/ethnic minorities who might respond differently to ART adjustments.
- Follow-Up Duration: Although 96 weeks is a respectable period for clinical trials, the long-term effects on inflammation and metabolic parameters might require even more extended monitoring. Some benefits or drawbacks may only emerge after several years.
- Missing Cellular Activation Markers: The study did not include a comprehensive assessment of cellular activation markers, which could have provided further insights into the subtle shifts in the immune system dynamics.
Recognizing these limitations is key. They remind us that the search for improved strategies in HIV management is ongoing, and that clinicians and researchers must continue to dig into these challenging issues with a critical eye. It also highlights the importance of designing future studies that can take a closer look at these hidden complexities.
Future Directions: Charting a Course for Better Outcomes
Given the modest changes observed in both systemic inflammation and metabolic parameters, it is clear that simply swapping one contemporary ART regimen for another may not sufficiently address the nerve-racking challenges of inflammation-driven comorbidities in HIV. The study emphasizes that alternative strategies—in tandem with ART adjustments—are essential.
Looking ahead, several key areas deserve attention:
- Adjunctive Therapies: Exploring anti-inflammatory agents or targeted immunomodulatory therapies that can work alongside traditional ART may provide the extra push needed to reduce systemic inflammation effectively.
- Personalized Medicine: Tailoring treatment based on a patient’s unique metabolic profile and inflammatory status could help in managing the subtle details that vary from one individual to another. Future research can focus on identifying biomarkers that predict who might benefit most from certain adjunct treatments.
- Integrated Lifestyle Interventions: Increasing emphasis on diet, exercise, and stress management presents a promising avenue. Coupling these lifestyle modifications with ART may offer compounded benefits, making this a super important area for long-term studies.
- Diverse Patient Populations: Ensuring that future studies have a more diverse participant base will help uncover any fine shades of response across different demographic groups, creating a more inclusive understanding of HIV management.
Each of these avenues represents a stepping stone toward a more comprehensive approach to treating HIV—one that acknowledges both the apparent successes in viral suppression and the hidden challenges of systemic inflammation and metabolic health.
Comparative Analysis: Dual vs. Triple ART Regimens
To simplify and organize the complex pieces discussed above, consider the following comparison between continuing dual ART and switching to a triple ART regimen:
| Parameter | Dual Therapy (DTG/3TC) | Triple Therapy (BIC/FTC/TAF) |
|---|---|---|
| Virologic Suppression | Maintained (>95%) | Maintained (>95%) |
| Inflammatory Biomarkers | Stable | Stable |
| Metabolic Parameters (Weight, Lipids) | Slight weight gain; minimal lipid changes | Slight weight gain; minimal lipid changes |
| Renal Function | Stable (eGFR steady) | Stable (eGFR steady) |
| Adverse Events | Low frequency; mostly grade 1-2 | Slightly higher frequency of mild drug-related effects |
By juxtaposing these two treatment strategies, it becomes apparent that while both regimens are effective at maintaining viral suppression, neither offered a marked advantage in decreasing systemic inflammation or improving metabolic outcomes. This table underscores the importance of looking beyond the primary endpoint of viral suppression when considering overall patient health.
Expert Opinions: What Does This Mean for Everyday Practice?
For healthcare professionals working in the field of HIV management, these findings are a reminder to work through the layered issues of treatment adjustments rather than relying exclusively on changes in drug regimens. Several expert opinions have started to shape the evolving approach:
- Individualized Treatment Plans: Given that both regimens maintained excellent viral control, the decision to switch should be based on the patient’s broader medical history and concerns—particularly in terms of comorbid conditions and quality of life.
- Integration of Complementary Strategies: Experts stress the importance of integrating nutritional counseling, regular physical activity, and stress management techniques as part of the overall treatment framework to help manage the subtle details of systemic inflammation.
- Ongoing Monitoring: Even though the differences in inflammatory biomarkers were negligible over 96 weeks, regular monitoring remains key. Clinicians are encouraged to keep a close eye on inflammatory and metabolic parameters over longer periods so that any emerging patterns can be addressed promptly.
These expert opinions push us to recognize that while medication is vital, the off-putting twists and turns of HIV management extend beyond pharmacotherapy alone. Ultimately, the research encourages a broader, more holistic approach—one where the integration of lifestyle modifications, psychological support, and innovative adjunctive therapies can form the backbone of patient care.
Long-Term Outlook: Steering Through an Evolving Landscape
As we look to the future, the landscape of HIV treatment continues to evolve. With every new study and clinical observation, clinicians are offered another chance to figure a path that addresses the layered issues of HIV management—from ensuring robust viral suppression to handling systemic inflammation and metabolic shifts.
Emerging trends and future directions include:
- The Role of Inflammation Modulators: Further research is needed to identify compounds or strategies that specifically target the tangled issues of immune activation and systemic inflammation. Novel therapies may eventually be used alongside ART to reduce the risk of cardiovascular and other inflammation-driven complications.
- Precision Medicine: There is growing anticipation that personalized treatment strategies will further refine the management of HIV, ensuring that each patient’s unique characteristics and risk factors guide therapy choices.
- Collaborative Care Models: The future of HIV management is set to benefit from a more integrated approach involving a range of healthcare professionals—from infectious disease specialists and endocrinologists to nutritionists and mental health experts—working together to manage the small distinctions that can significantly impact long-term health outcomes.
In summary, the study on switching from DTG/3TC to BIC/FTC/TAF reminds us that once viral suppression is achieved, further refinements in drug therapy may not be the silver bullet for addressing the confusing bits of systemic inflammation. Instead, the results urge the clinical community to embrace a multi-dimensional approach, one that supports patients both medically and emotionally over the long haul.
Conclusion: Taking the Wheel in HIV Management
In conclusion, the INSTINCT/GESIDA10918 study offers valuable insights for those charged with managing HIV care. The trial’s findings highlight that both dual and triple ART regimens maintain robust viral suppression but yield limited differences in systemic inflammation and metabolic outcomes over a period of 96 weeks. For clinicians, this serves as a reminder that switching antiretroviral therapies—even to a seemingly more comprehensive regimen—may not automatically resolve the complicated pieces of chronic inflammation.
Instead of expecting dramatic shifts in systemic inflammatory markers, healthcare providers should consider adopting broader management strategies that include anti-inflammatory adjuncts, dietary adjustments, exercise routines, and stress reduction techniques. As we continue to grapple with the intertwined challenges of HIV, inflammation, and metabolic health, a balanced and patient-centered approach remains key. This means taking the wheel, managing your way through the subtle details, and steering through the fine points with an open mind to evolving therapeutic innovations.
For patients and clinicians alike, these findings are a call to action: broaden the focus beyond viral suppression alone and invest in comprehensive care that addresses both the obvious and hidden complexities of HIV treatment. Although the path may be full of confusing bits and nerve-racking uncertainties, ongoing research and a commitment to holistic care will help light the way forward in the ever-evolving landscape of HIV management.
Ultimately, embracing alternative strategies—be it through lifestyle changes, targeted anti-inflammatory treatments, or personalized medicine—can bridge the gap left by ART regimen switches. By acknowledging and addressing both the tangible and subtle aspects of treatment, we can continue to improve patient outcomes and move closer to a future where the overall burden of HIV is significantly reduced.
As the clinical community dig into these challenging issues, continued dialogue and innovation are critical. Let this study serve not as an endpoint, but as an impetus to explore the multi-dimensional facets of HIV care—helping to ensure that every patient’s journey is guided by an integrated, effective, and compassionate approach.
Originally Post From https://www.endocrinologyadvisor.com/news/systemic-inflammation-in-suppressed-hiv-similar-after-switch-to-3-drug-art/
Read more about this topic at
Why does chronic inflammation persist: An unexpected role …
Understanding acute and chronic inflammation