Rising Trends in Alternative Health Plans Amid Soaring Healthcare Costs
The landscape of health insurance is undergoing a noticeable transformation. Many employers are rethinking their traditional benefits packages and looking into alternative health plans that aim to simplify the tangled issues of modern healthcare costs while offering more affordable solutions. In today’s healthcare market, traditional recipes like HMOs, PPOs, and HDHPs are frequently seen as too complicated and overwhelming. This has steered many businesses toward exploring innovative models such as association health plans (AHPs) and individual coverage health reimbursement arrangements (ICHHRAs), in addition to emerging variable copay designs.
Employers and their healthcare partners are now tasked with figuring a path through tricky parts of rising medical expenses, which are loaded with issues related to affordability and effective cost management. The market, though still in its early stages on some fronts, signals a broader shift toward alternative strategies that could potentially reshape how benefits are delivered. As this transition continues, it is essential to understand both the opportunities and challenges left in the wake of these innovative plans.
Alternative Health Plans: A Fresh Perspective on Employer Benefits
Many employers are increasingly questioning the existing benefits structures due to the persistent escalation of healthcare costs. A growing number of studies and surveys indicate that employer-sponsored plans have become too expensive, given that healthcare costs have seen consistent jumps over the years. This frustration has spurred a move toward alternative health plans which aim to introduce affordability and simplicity to an otherwise intimidating system.
Alternative health plans are essentially new or reimagined insurance designs that are intended to provide clear cost measurements and help manage the confusing bits that characterize traditional plans. These innovative strategies help insurers and employers adjust to the rapidly evolving healthcare environment, where each twist and turn in the market demands keen attention to the fine points of plan design.
Exploring the Benefits of Association Health Plans (AHPs)
One key alternative approach gaining popularity is Association Health Plans (AHPs). These plans pool smaller companies and self-employed individuals together, allowing them access to the benefits typically reserved for larger groups. By joining forces, small employers can make their way through the maze of healthcare options and access more affordable benefits that are usually available through larger risk pools.
AHPs come with several notable advantages:
- Stable Cost Management: Pooling with other small businesses can help smooth out the unpredictable spikes in costs.
- Enhanced Benefit Customization: When small employers band together, they can negotiate for better benefits and reduced premium costs compared to operating individually.
- Increased Negotiating Power: Larger groups have the upper hand in discussions with insurers, often resulting in savings in the range of 8% to 18% compared to what small group policies might typically cost.
While the benefits of AHPs are enticing, employers must also be aware of potential limitations. For example, the range of benefits available in an AHP might not always include everything mandated in federally controlled marketplaces. Thus, businesses should carefully weigh the necessary coverage against what these alternative plans offer before making a final decision.
Diving Into Individual Coverage Health Reimbursement Arrangements (ICHHRAs)
Another alternative that is emerging on the healthcare scene is the Individual Coverage Health Reimbursement Arrangement (ICHRA). These are employer-funded plans designed to provide tax-free funds directly to employees. The money can be used to cover the premiums for individual health insurance or other qualified medical costs, offering employees more choice in selecting their coverage.
ICHRA benefits include:
- Cost Control: With employers funding these plans, there is greater transparency when it comes to determining how much employees need to pay out of pocket.
- Flexibility and Personal Choice: Employees get the freedom to choose individual insurance plans that best meet their personal and family needs.
- Emphasis on Technology: Many ICHRA providers are leveraging technological tools which simplify administrative burdens for small employers.
Even though ICHRAs offer multiple advantages, there remain several challenges. For instance, some employees might encounter a limited selection of individual plan options compared to traditional group plans. This reduced variety could be risky if employees require a broader network or specific types of coverage. Moreover, navigating the various choices available under ICHRAs can be full of problems, especially if system users are not well-versed in the little details of individual insurance policies.
Variable Copay Plans: Striking a Balance Between Cost and Quality
An emerging trend in alternative health plans is the design of variable copay models. These models are set to counter one of the biggest headaches in today’s healthcare setting: the unpredictable out-of-pocket costs that can often be intimidating for patients. With variable copay plans, the amount a patient must pay directly varies depending on factors like provider cost and the quality of services rendered. Essentially, the goal is to guide beneficiaries toward high-value providers that offer economical yet quality care.
Some key benefits of variable copay plans include:
- Cost Transparency: By adjusting copays based on provider performance and cost, these plans make the confusing bits of healthcare billing simpler and more predictable.
- Encouragement for Quality Care: Beneficiaries are incentivized to choose providers known for both affordability and high-quality service.
- Workable Simplicity: Although traditional plans often come with layers of administrative complications, variable copay plans focus on making things straightforward by clearly outlining patient responsibilities at the point of care.
Even with their apparent simplicity, variable copay plans come with hidden complexities. For example, if the criteria for determining copay amounts are not communicated effectively, employees might still feel left in the dark. Additionally, some plan participants might find the network too narrow or the cost structure too unpredictable during times of health emergencies or sudden changes in provider networks.
Understanding the Role of Communication and Education in Alternative Health Plans
One of the recurring themes in the shift toward alternative health plans is the importance of conversation and clear communication. Many beneficiaries, as well as the HR teams managing these benefits, find the health benefit system intimidating simply because of its twisted procedures and the overwhelming amount of tangled details. Employers must take the wheel in working through these challenges by investing time and resources into educating employees about new options.
Key areas of focus include:
- Benefit Communication Strategies: Explaining the unique aspects of AHPs and ICHRAs through simple language helps demystify the process.
- Employee Education Programs: Workshops, online modules, and one-on-one counseling sessions can assist employees in making informed decisions about their healthcare options.
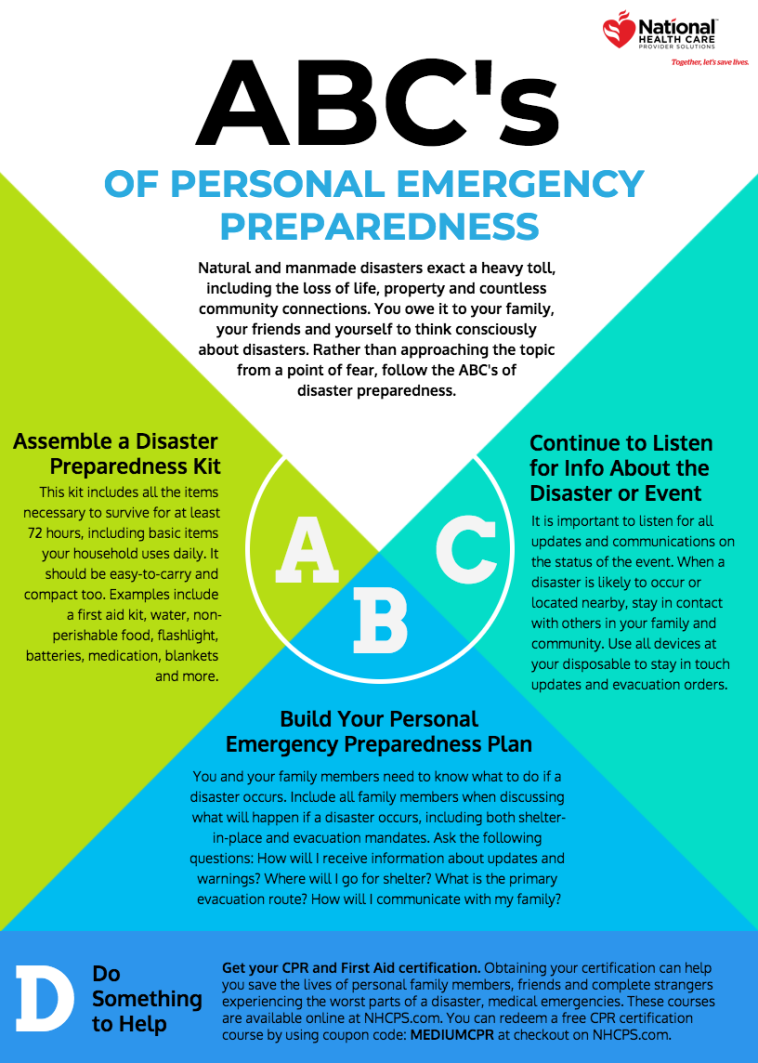
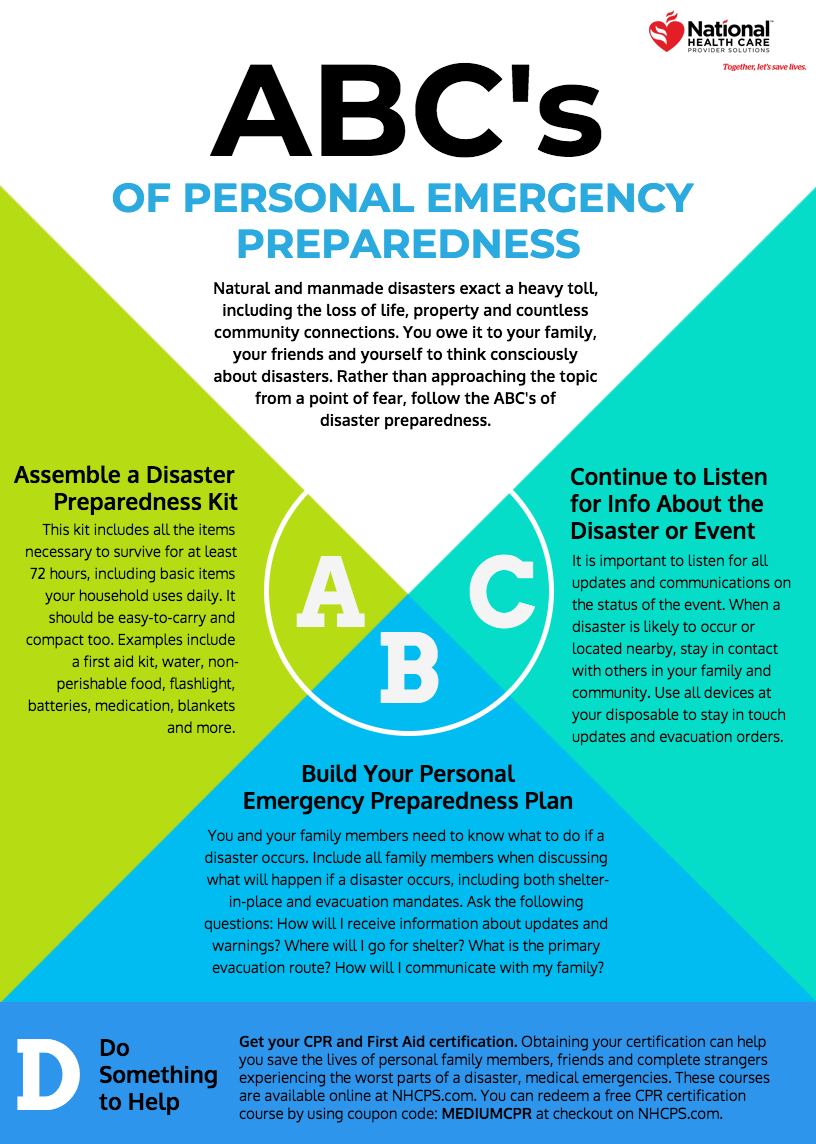
- Clear Presentation of Costs: Using tables, infographics, and simple equivalence charts can help employees understand variable copay structures and related responsibilities.
For instance, the use of clear cost tables can demystify the amount an employee might be required to pay, ensuring that there is minimal confusion when it comes to understanding health expenses. When employees see a straightforward breakdown, they are more likely to embrace and utilize their benefits effectively.
Breaking Down the Tricky Parts: Employer Strategies for Managing Rising Healthcare Costs
Recent surveys, such as the Employer Health Care Strategy Survey, paint a stark picture: healthcare costs have surged dramatically, with projections indicating that costs could be as much as 62% higher than a few years ago. This scenario is tense and filled with challenges for both employers and insurers, leading many to explore bolder moves to tackle these upward spirals in expense.
Employers are now thinking of themselves as healthcare population strategists rather than just benefits managers. This evolution in mindset is critical because it shifts the focus to a broader, more integrated understanding of employee well-being that encompasses not only physical health, but also mental and behavioral healthcare needs.
Strategies that employers may consider are:
- Long-Term Cost Modeling: Developing projections based on both current expenditures and future trends to help manage unexpected spikes.
- Partnerships With Insurers: Engaging in closer collaboration with carriers to design tailored alternative plans that account for both affordability and quality.
- Enhanced Wellness Programs: Integrating comprehensive wellness initiatives that target preventive care, which in turn can reduce emergency-related expenses.
By embracing these steps, employers can effectively figure a path through the challenging parts of rising healthcare costs, while also delivering meaningful value to their employees. Strategic planning and a proactive approach can transform what was once a nerve-racking situation into an opportunity for positive change in the benefits landscape.
Assessing the Small Business Impact: Alternative Health Plans for the Under-Served
Small businesses have long grappled with the off-putting high costs of employee health benefits. Traditional small group markets, often riddled with tension due to narrow risk pools and limited negotiating power, leave little room for budget flexibility. Association health plans provide a solution by aggregating small employers into larger risk pools that mirror the stability and benefits of a large group plan.
For small business owners, the benefits of alternative health plans include:
- Collective Bargaining Power: Pooling together means more leverage with health plans and better-aligned cost reductions.
- Customizable Benefits: Smaller employers have the opportunity to tailor benefit packages to better suit their unique workforce needs.
- Simplified Administration: Technologically-enabled solutions can alleviate the burdens of traditional plan management.
However, small employers must take a closer look at the fine shades in any plan design to ensure that essential coverages, such as preventative care and mental health services, are not left behind. The transition to alternative models requires careful scrutiny of the detailed components of any proposed plan so that employees receive comprehensive protection without unexpected exclusions.
Lessons from Industry Leaders: How Providers and Insurers Are Adapting
Prominent players in the health insurance industry, like leading commercial health plan executives, are carefully watching the evolving market. Their insights provide useful clues as companies gear up to address both rising costs and shifting consumer demands.
Key observations include:
- Risk Pool Management: Insurers are examining whether moving members between different benefit pools can be financially sustainable over the long term.
- Market Consolidation: With new vendors entering the market, consolidation seems inevitable. This means that over time, a clearer picture will emerge as winners and more integrated partnerships form.
- Use of Advanced Technology: Many carriers are testing digital solutions that streamline administrative tasks while making cost structures transparent. Such technological innovations are critical in easing the overwhelming process of managing health benefits.
These approaches underscore the need for ongoing dialogue and continuous re-evaluation of plan designs. Insurers, employers, and even employees need to be open to adjustments and improvements as the healthcare benefit ecosystem shifts. According to industry leaders, the market is still in a transitional phase where the opportunities to save money and improve care delivery are significant, provided that all parties are willing to take a closer look at the subtle parts that differentiate one model from another.
Charting a Future Path: Strategic Considerations for Payers and Employers
The rapidly evolving alternative health plans environment necessitates that both payers and employers re-think their long-term strategies. With costs projected to rise and consumer expectations shifting, the need for a more strategic alignment between health plans and employer offerings has never been more critical.
In this regard, several considerations emerge:
- Partnering for Innovation: Both employers and insurers must work together to design plans that prioritize not just cost savings but also accessible, quality care. This might include partnerships with tech providers who can help reduce the nerve-racking administrative burdens on HR teams.
- Regular Plan Reassessment: Given that policies and regulations may change as the market consolidates, it is key for businesses to review and possibly revise their plan options in regular cycles, ensuring that they remain aligned with both legislative developments and employee needs.
- Flexibility and Scalability: Plans that offer modular designs allow employers to add or remove benefits without a complete overhaul. Flexibility is especially important in a market where the fine shades between different options can have significant financial consequences.
Employers who approach these decisions as ongoing processes, rather than one-time changes, are better positioned to manage the expensive and sometimes intimidating shifting marketplace. By being proactive and embracing dynamic strategies, businesses can help ensure the longevity and sustainability of their benefits packages.
Comparative Insights: A Table of Alternative Health Plan Options
For a clearer understanding of how alternative health plans compare, consider the following table outlining key factors related to AHPs, ICHRAs, and variable copay plans:
| Key Factor | Association Health Plans (AHPs) | ICHRA (Individual Coverage Health Reimbursement Arrangements) | Variable Copay Plans |
|---|---|---|---|
| Cost Stability | Larger risk pools can lead to more stable costs | Employer-funded with transparent budgeting | Copays adjust based on provider quality and cost |
| Customization | Flexible benefit packages through group bargaining | High individual flexibility in choosing plans | Tailored to incentivize both affordability and quality |
| Administrative Simplicity | Shared administrative responsibilities among small groups | Enhanced by technology-backed solutions | Clear cost breakdown reduces confusion at the point of service |
| Risk Considerations | May exclude federally mandated benefits | Limited plan options for specialty needs | Varies by provider; could narrow network choices |
This table illustrates how each alternative plan addresses various aspects of healthcare management. While no single plan is perfect for every employer, understanding these differences can help businesses make informed decisions and weed through the tangled issues of traditional healthcare policy.
Charting a Course Through Tricky Parts: Practical Tips for Employers
Adopting alternative health plans is not as straightforward as flipping a switch; it requires methodical planning and careful attention to every twist and turn along the way. For employers looking to invest in this new approach, here are some practical tips to consider:
- Do Your Homework: Take a closer look at the detailed offerings of different plans and ask providers to explain the nitty-gritty elements that differentiate one plan from another.
- Engage Stakeholders: Work with HR, finance teams, and even employee focus groups to understand which aspects of benefits matter the most. Their input is key to managing the subtle parts of any proposed changes.
- Invest in Education: Organize training sessions or digital modules that help employees figure a path through the confusing bits of healthcare options, including discussing how variable copays work in practice.
- Monitor and Adjust: The healthcare market is dynamic. What works well today may need to be tweaked in the future. Regularly assess the performance of your benefit plans and make modifications as necessary.
By following these guidelines, employers can better manage the challenging parts of rising healthcare costs while keeping employee satisfaction high. A proactive strategy not only benefits the organization’s bottom line but also ensures that employees feel confident and secure about their benefits.
The Role of Technology in Simplifying Alternative Benefit Models
Technology is playing an essential role in untangling the tricky parts of modern healthcare plans. From digital platforms that simplify benefits enrollment to analytics tools that help forecast future expenses, tech innovations are proving to be a game changer in this field. Many companies that offer ICHRAs, for example, emphasize the role of technology in streamlining administration and reducing the nerve-racking burden of manual processing.
Some of the technological advancements that are making a difference include:
- Automated Enrollment Systems: Simplify the process of signing up for new plans, reducing the chance of errors and saving time for both employers and employees.
- Real-Time Cost Analysis: Tools that break down the fine details of cost-sharing, helping beneficiaries see at a glance what their expenses might look like at various providers.
- Digital Communication Platforms: These ensure that employees receive timely updates about benefits changes, policy improvements, and important deadlines—a critical aid when benefits systems can often feel overwhelming.
- Interactive Benefit Calculators: Allow users to run scenarios and explore how different plan elements, like copays, might shift based on provider choice or usage patterns. This interactive approach demystifies the complicated pieces of traditional healthcare plans.
The infusion of technology not only helps companies cut down on administrative hassle but also makes it easier for employees to steer through alternative benefits. With better data at hand, decision-makers can fine-tune their offerings, ensuring that the investments made in alternative health plans are both cost-effective and user-friendly.
Potential Challenges and Points of Caution in the Transition
Despite the promising outlook, transitioning to alternative health plans is not without its challenges. Many aspects of this process can appear overwhelming if not carefully managed. For instance, when moving from traditional group plans to alternatives like AHPs or ICHRAs, employers must keep in mind:
- Limited Provider Networks: Some alternative plans may offer fewer provider choices, which can result in employees having a harder time finding the care they need.
- Regulatory Uncertainty: As state and federal policies continue to evolve, there is a constant need to stay updated on compliance matters that can affect plan design and operation.
- Employee Adaptation: The switch to models like variable copay plans may be intimidating for some employees, particularly if they are accustomed to the predictability of traditional co-insurance models.
Mitigating these risks involves careful planning, transparent communication, and ongoing support. Employers must ensure that changes are phased in gradually and that employees have ample opportunities to ask questions and become familiar with new processes. This proactive approach helps reduce the chance of confusion and builds trust in the new system.
Evaluating the Overall Impact: A Balanced Perspective
In the final analysis, the shift towards alternative health plans reflects a broader trend in the healthcare industry—one that values both innovation and cost control. While these new strategies offer promising solutions to manage rising costs and simplify benefits delivery, they also require a careful balance between flexibility and adequate coverage.
On one side, alternative models provide potential for significant savings and better risk pooling. By leveraging technology and innovative plan designs, employers can reduce their healthcare expenditures while offering competitive and customizable benefits to their workforce.
Conversely, it is essential to be aware that these approaches may also introduce certain risks. Plans that narrow provider networks or exclude mandatory benefits can leave employees vulnerable, especially if they do not fully understand the small distinctions between the options available. Ultimately, the success of any alternative health plan depends on how well employers and payers work together to manage the intricate dance between cost, coverage, and user-friendly design.
Final Thoughts: Embracing Change in a Changing Healthcare Landscape
The world of healthcare is shifting rapidly, and alternative health plans stand at the forefront of this transformation. Whether it’s through the pooled benefits of association health plans, the flexibility of individual coverage health reimbursement arrangements, or the clarity offered by variable copay plans, employers have more choices than ever before in designing benefit packages that align with today’s economic realities.
This period of change is both exciting and challenging. As businesses confront the overwhelming pressures of rising costs and the countless twists and turns of regulatory changes, embracing innovative benefit ideas can offer a ray of hope. It is important, therefore, for all stakeholders—from employers and HR teams to insurers and employees—to collaborate closely and remain open to fresh, inventive solutions.
By taking the time to dig into the fine points of different plan options, investing in technology and education, and continuously re-evaluating strategies, companies can not only manage the rising costs but also build a more resilient, transparent, and effective benefits system. Through these efforts, the healthcare sector can progress toward a future where both affordability and quality are seen as complementary rather than mutually exclusive.
In conclusion, while the journey to fully integrate alternative health plans is loaded with challenges, it is also a path filled with opportunities. As the market matures, and as both employers and payers adjust their strategies, we can expect a more sustainable, accessible, and transparent benefits landscape—a landscape that truly meets the needs of all participants.
Employers must keep an open mind and be willing to make adjustments as they figure a path through these tricky parts. With clear communication and systematic planning, the shift towards alternative health plans can pave the way for innovative, cost-efficient solutions that benefit everyone involved in the healthcare ecosystem.
Ultimately, the key to success lies in partnership, innovation, and a commitment to continuous learning. Stakeholders must not only embrace new methods but also strive to understand the little twists and hidden complexities behind every decision. By doing so, businesses can secure a future where healthcare is both affordable and of high quality, ensuring that employees are well cared for and that the system remains sustainable for years to come.
Originally Post From https://www.techtarget.com/healthcarepayers/feature/Breaking-down-the-ABCs-of-rising-alternative-health-plans
Read more about this topic at
Reimagining health care: How two systems are leading the …
Reimagining the Health System