Revisiting the Case: When Timely Diagnosis Turns the Tide in Autoimmune Illness
The story of a 73‐year‐old English gentleman who came into the emergency department with shortness of breath and signs of kidney troubles is more than just a clinical case—it is an opinion piece on the value of keeping a wide eye when assessing health challenges. In the modern era of medicine, where cases can get tangled with tricky parts and overwhelming twists and turns, this patient’s journey reminds us how essential it is to figure a path through confusing bits and to treat each sign as a key clue in a larger puzzle.
Unpacking the Puzzle: Recognizing Autoimmune Disorders Beyond the Obvious
Every medical practitioner has faced situations where symptoms mimic common infections but in reality hide a more complex condition. This case of acute kidney injury (AKI) masked behind a chest infection is an excellent example of how the subtle parts of a patient’s presentation can hide a dangerous twist. It shows that while lower respiratory tract infections and pneumonia are common, one must always get into the finer details when these conditions strike suddenly in the elderly.
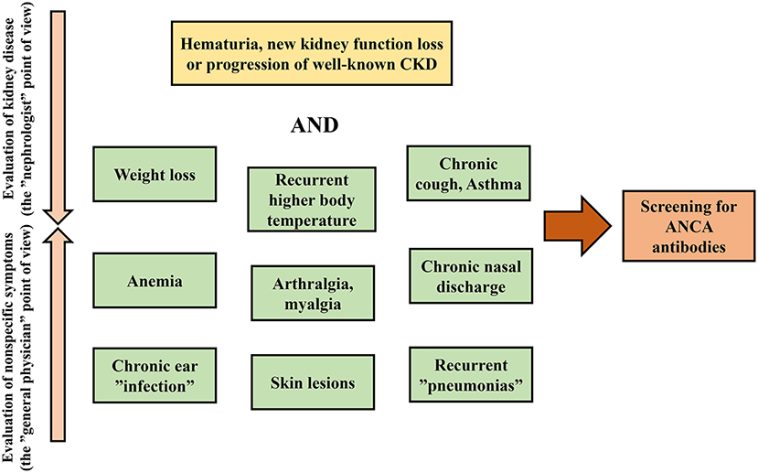
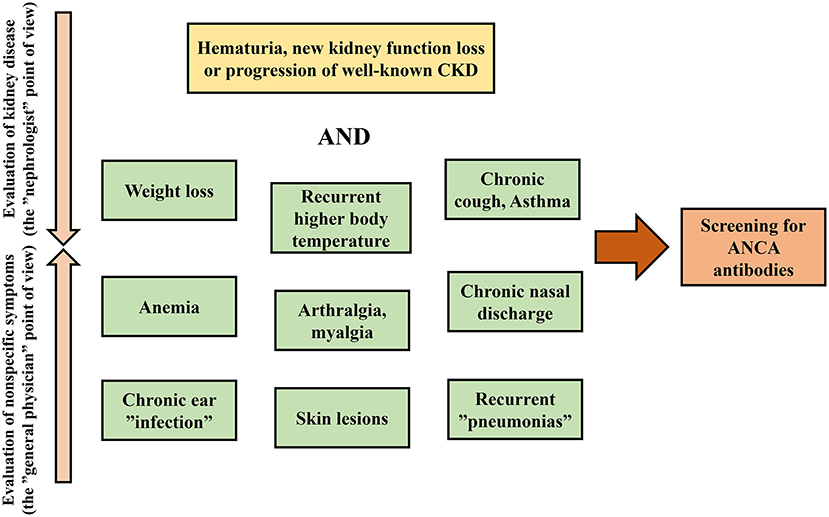
It is super important to remember that autoimmune disorders like antineutrophil cytoplasmic antibody (ANCA)‐associated vasculitis are full of problems that demand both speed and precision during diagnosis. As clinicians steer through symptoms like cough and shortness of breath, suddenly finding abnormal blood tests and chest imaging can make one pause and dig into the possibility of an underlying autoimmune process. The challenge is not just recognizing these signs but also managing your way through the treatment options in order to avoid any irreparable damage.
Symptoms as Signposts: Learning from the Patient’s Presentation
At first glance, shortness of breath and bloody cough might easily be chalked up to severe pneumonia. However, this case underscores that even when symptoms appear straightforward, they might conceal a layered story of autoimmune aggression. The patient’s history, physical exam, and bedside tests such as urine dipstick analyses played a key role in highlighting the hidden complexities of his condition.
Observing details like the presence of blood and protein in the urine should alert any savvy practitioner to consider the possibility of renal involvement in systemic conditions. In our case, it was the strong reaction on the urine dipstick that spurred a further autoimmune screen, ultimately pointing to granulomatosis with polyangiitis—a subtype of ANCA-associated vasculitis. His scenario teaches us the value of staying alert and considering every little twist when symptom presentations seem standard but are actually loaded with issues.
Deep Diving into the ANCA-Associated Vasculitis Landscape
ANCA-associated vasculitis (AAV) is a complex group of autoimmune conditions where the immune system mistakenly attacks the small and medium-sized blood vessels. In this disorder, the body’s defense cells, such as neutrophils, turn against their own tissues. When these neutrophils are triggered by autoantibodies, the resulting inflammation and damage can involve many organ systems—from the heart and kidneys to the lungs and nervous system.
In our patient’s situation, the detection of proteinase 3-positive (PR3+) ANCA was a smoking gun that gave direction to the diagnosis. This case underscores that medicine is not always clear-cut; sometimes the key to breakthrough lies in insulting the more tangled issues of the immune system.
For a better understanding, here are some of the small distinctions that make a difference in diagnosing AAV:
- Understanding the triggers: Genetic predispositions, responses to injury, and certain drugs can stir the immune system.
- Identifying clinical patterns: Symptoms may evolve quickly, moving from acute presentations to chronic phases in just days.
- Monitoring laboratory values: Elevated inflammatory markers, abnormal urine, and changes in kidney function are central to the diagnosis.
This detailed approach highlights the key fact that every abnormal finding is like a breadcrumb leading clinicians closer to the real problem lurking behind common presentations.
Timely Intervention: A Lifeline in a Race Against Time
Time is of the essence when it comes to conditions like AAV, where each minute of delay may result in irreversible organ damage. In this case, the patient’s clinical course was nerve-racking yet full of hope after the prompt initiation of treatment. The rapid use of immunosuppressive medications such as steroids, along with plasmapheresis to clear out the ANCA antibodies, played a monumental role in stabilizing his condition.
Here are some bullet points to illustrate the treatment options and why early intervention is super important:
- High-dose steroids: Immediate administration of intravenous methylprednisolone helped control the overwhelming immune attack.
- Immunosuppressive drugs: The addition of cyclophosphamide, coupled with a carefully planned tapering course of oral prednisolone, demonstrated how essential early and aggressive immunosuppression is.
- Plasmapheresis sessions: Using plasmapheresis to physically remove harmful antibodies added another level of protection for critical organs such as the kidneys.
This multi-pronged approach ensured that the tricky parts of the patient’s condition were managed early enough to prevent long-term damage—teaching us that in modern medicine, timely, multi-modal intervention is not just beneficial, it is necessary.
Lessons Learned from a Real-World Case Presentation
The narrative of this patient’s medical journey provides a stepping stone for reflection in everyday clinical practice. When conventional symptoms present in an off-putting manner, there is a fine line between routine treatment and discovering life-threatening diseases. Let’s take a closer look at the key lessons from this case:
- Keep a Broad Differential:
Even when the signs point toward a straightforward pneumonia, consider that the roots of the problem may be tangled with autoimmune processes. Early lab tests such as the urine dipstick and detailed serological testing help unmask underlying issues.
- Importance of Imaging:
Chest X-rays and CT scans offered invaluable clues. The typical batwing appearance and bilateral consolidation on imaging—when placed in the right clinical context—should alert clinicians to the possibility of alveolar hemorrhage or underlying vasculitis.
- Interdisciplinary Collaboration:
This case called for a seamless transition between emergency care, intensive care, and specialized rheumatology follow-up. In today’s world, finding your path through interdisciplinary care is super important for harnessing cumulative expertise.
Such reflections not only validate the time-critical nature of diagnosis in autoimmune vasculitis but also highlight the importance of being flexible and observant in our treatment approaches.
Understanding the Hidden Complexities: The Role of Laboratory Testing
The pathway to an accurate diagnosis in autoimmune disorders is paved with a host of little details. Laboratory tests are not mere numbers; rather, they represent the delicate balance between a healthy immune response and an attack on one’s own tissues.
Let’s break down the lab findings in our case:
| Test | Result | Normal Range | Interpretation |
|---|---|---|---|
| Hemoglobin (Hb) | 7.7 mmol/L | 8.6–11.2 mmol/L | Below normal, suggesting anemia |
| White Cell Count (WCC) | 12.9 x 10⁹/L | 4.0–11.0 x 10⁹/L | Elevated, hinting at an inflammatory or infectious process |
| Neutrophils | 11.12 x 10⁹/L | 2.0–7.5 x 10⁹/L | Markedly elevated, supports infection or significant inflammation |
| C-Reactive Protein (CRP) | 152 mg/L | < 0.3 mg/dL | Significantly raised, indicating a strong inflammatory response |
| Creatinine | 153 µmol/L | 62–115 µmol/L | Elevated, pointing to kidney impairment |
| D-Dimer | 5,884 ng/mL | <500 ng/mL | Significantly elevated, consistent with severe inflammation |
This table not only outlines the patient’s abnormal laboratory markers but also serves as a reminder of how each elevated or decreased value may be a signal to poke around further when assessing a patient. Recognizing each of these key laboratory findings is akin to piecing together a puzzle where every marker has its hidden meaning.
Treating the Challenge: Steering Through Therapeutic Options
When the immune system turns against its own body, the treatment strategy must be as multifaceted as the illness itself. In the context of ANCA-associated vasculitis, a prompt and aggressive approach involving a combination of high-dose steroids, immunosuppressive therapies, and plasmapheresis is often the only way to arrest the immune attack and preserve organ function.
For our patient, the treatment strategy included:
-
Immediate Intervention:
The administration of a high-dose intravenous steroid gave an immediate boost to counter the inflammation.
-
Controlled Immunosuppression:
The subsequent prescription of cyclophosphamide combined with a tapering schedule of prednisolone illustrated the delicate balance of immunosuppression required to achieve remission.
-
Supportive Therapies:
Seven sessions of plasmapheresis were utilized to lower the levels of circulating antibodies, thereby mitigating further immune damage.
This layered approach is instructive for practitioners: when the stakes are high, it is essential to get into the little details of treatment regimens and tailor interventions accordingly. Each treatment modality complements the other, creating a synergy that ultimately gives patients the best chance at recovery.
Looking at the Bigger Picture: The Intersection of Kidney and Pulmonary Care
The interplay between the kidneys and lungs in patients with ANCA-associated vasculitis is one of the fine shades that make this field particularly challenging. In many cases, involvement of these organs can steer the prognosis and dictate the urgency of intervention. As seen in this case, lung imaging revealed bilateral pulmonary consolidations that resembled several potential causes including pulmonary edema, hemorrhage, or even viral pneumonia.
However, when seen in tandem with impaired kidney function, the imaging findings shifted the clinical suspicion towards an underlying vasculitis process. The convergence of abnormal test results—for both respiratory and kidney systems—illustrates just how key it is for clinicians to work through multiple angles rather than making quick assumptions based solely on one system’s findings.
In practice, managing such patients involves:
-
Careful Radiological Analysis:
The central batwing appearance on CT scans and diffuse consolidations point to a pattern that can, with the right clinical input, suggest immune-mediated hemorrhagic processes.
-
Close Laboratory Monitoring:
Tracking the trends in creatinine and inflammatory markers reminds us that the kidneys often serve as early indicators of systemic immune activation.
-
Coordinated Care Teams:
Effective management relies on the collaboration of pulmonologists, nephrologists, and rheumatologists who together can piece out the finer details of the presentation.
The Role of Follow-Up and Continuous Monitoring
Recovery from aggressive conditions like ANCA-associated vasculitis requires more than just initial crisis management. Long-term follow-up, careful adjustment of medications, and repeated imaging studies are all part of ensuring a full recovery. In our patient’s journey, a follow-up chest X-ray at four months revealed significant improvement, underscoring that sustained monitoring can help confirm the success of the chosen treatment strategy.
Key takeaways for post-discharge care include:
- Regular Imaging: Routine chest X-rays or CT scans can help track changes in lung consolidation or the resolution of any abnormal patterns.
- Laboratory Surveillance: Continuous tracking of kidney function markers such as creatinine and eGFR ensures that any emerging issues can be spotted early.
- Clinical Assessments: Frequent follow-up visits create opportunities for practitioners to get around any lingering symptoms and adjust the therapeutic regimen.
This ongoing care strategy is a reminder that the journey toward health is often a marathon rather than a sprint, and each checkpoint is essential in ensuring lasting recovery.
Reflections on the Broader Implications for Modern Medicine
The case of our patient has broader implications than just the experience of one individual—it prompts an opinion on how modern medicine can better address conditions that are full of tricky parts and tangled issues. In a time when diagnostic capabilities and treatment protocols are constantly evolving, maintaining a vigilant and holistic mindset is indispensable.
Some of the higher-level considerations include:
-
Enhanced Diagnostic Training:
Medical curricula and continuing education should emphasize the importance of recognizing subtle signs that may indicate complex autoimmune conditions.
-
Interdisciplinary Collaboration:
Collaboration among various specialists should be super important. By bridging the knowledge from different fields, clinicians can piece together the hidden complexities of a patient’s presentation more effectively.
-
Patient-Centered Approaches:
Treating conditions such as AAV is not only about managing the immediate crisis but also about engaging patients in long-term care strategies. Educating patients about their condition, the rationale behind treatments, and the importance of follow-up is a must-have strategy in ensuring adherence and better outcomes.
When we look at the challenges from a broader perspective, what emerges is a landscape where even the smallest oversight can lead to delayed diagnosis and poorer outcomes. This case is a prime example of why every laboratory result, every imaging finding, and every clinical sign must be interpreted within a wider, more integrated framework.
Bridging Modern and Alternative Treatments in Autoimmune Conditions
While this case emphasizes the strength of modern medical interventions like immunosuppressive therapy and plasmapheresis, it also opens up a conversation on the potential role of complementary health approaches. Alternative medicine and nutritional support can serve as supportive pillars alongside conventional treatment to help manage side effects and improve overall well-being.
For example, nutritional strategies have been reported to help reduce inflammation and strengthen the immune system. Though not a replacement for aggressive immunosuppressive therapy, nutritional counseling and lifestyle modifications can work as adjunct treatments, helping to balance out the full spectrum of recovery needs.
Points to consider include:
-
Anti-Inflammatory Diets:
Foods rich in omega-3 fatty acids, antioxidants, and vitamins play a role in calming an overactive immune system. Diets focusing on fruits, vegetables, and whole grains may offer super important benefits during recovery.
-
Mind-Body Practices:
Techniques such as meditation and yoga can help manage stress levels—a factor that can otherwise complicate immune-mediated conditions. Reducing stress helps the body stay balanced during recovery.
-
Physical Rehabilitation:
Gentle exercise and physiotherapy are key in restoring mobility and function, particularly when patients have been debilitated by an acute illness.
By embracing both modern medicine and supportive alternative approaches, clinicians offer patients a more holistic outlook on recovery—one that caters not just to the physical but also to the mental and nutritional well-being of each individual.
Patient Stories and the Human Element in Healthcare
Beyond laboratory values and imaging studies, every case tells a human story. The account of this patient is a reminder that behind every set of numbers and test results lies a life full of hopes, challenges, and the quiet resilience required to bounce back from a serious illness.
The patient’s journey—from arriving in the emergency department with overwhelming symptoms to receiving coordinated care that preserved his vital organs—sheds light on the importance of integrating empathy into clinical practice. It is one thing to treat a patient’s lab abnormality; it is another to support someone through a nerve-racking medical crisis with both expert care and human kindness.
For healthcare providers, this case reinforces the need to:
- Embrace Empathy: Listening carefully to patient histories, understanding their anxieties, and reassuring them during treatments are all part of effective care.
- Blue-Sky Thinking: Innovate continuously by integrating both technological advancements and compassionate care to address all facets of patient health.
- Communicate Clearly: Using layman’s terms to explain complex interventions ensures that patients are true partners in their recovery process.
The human element is perhaps the most super important aspect of all medical interventions. It is the gentle bridge between advanced clinical practice and compassionate care, ensuring that no patient ever feels lost in the maze of treatments and tests.
Advocacy for Awareness and Research in Autoimmune Diseases
Cases like this highlight the need for ongoing research and increased awareness about autoimmune conditions. While advances in diagnostic techniques have made it easier to pick up on subtle cues, there is still a significant amount of work to be done when it comes to understanding the full spectrum of immune disorders. Continuing to support research not only improves diagnostic accuracy but also fosters the development of newer, more effective treatment protocols with fewer side effects.
Advocacy in the following areas is key:
-
Enhanced Funding:
Allocating more resources to autoimmune research can lead to breakthroughs that refine our approach to treatment, ensuring that fewer patients face the nerve-racking progression of untreated disease.
-
Educational Outreach:
Seminars, workshops, and online platforms should be used to educate both healthcare professionals and the public on the early signs of conditions like ANCA-associated vasculitis.
-
Collaboration Across Fields:
Bringing together experts in immunology, nephrology, pulmonology, and even alternative medicine can foster an environment where the full spectrum of the disease is understood and managed effectively.
This advocacy is not merely academic—it directly translates into better patient care by ensuring that clinicians have the super important tools and knowledge to act swiftly and accurately when faced with the subtle details of an autoimmune crisis.
Conclusion: Finding Your Way Through the Maze of Autoimmune Diagnostics
In reflecting on the story of this patient, it becomes clear that the journey through autoimmune disorders is filled with tricky parts, tangled issues, and nerve-racking moments. Yet, by recognizing each subtle detail—from abnormal lab values to unusual imaging findings—clinicians can figure a path that not only saves lives but also enriches our understanding of how best to treat these conditions.
This case is a prime reminder that when symptoms seem common but lab results paint a different story, it is super important to think broadly and act quickly. The patient’s remarkable recovery within a couple of weeks underscores that early, aggressive management can transform a tense clinical scenario into a story of hope and recovery.
As we continue to navigate the ever-changing maze of modern medicine, let us remember that every patient is a testament to the need for careful observation, prompt intervention, and above all, compassionate care. Building our practices around these principles ensures that we do not merely treat disease but truly help our patients thrive—and that is the real win in the battle against complex autoimmune disorders.
While the journey may be riddled with challenges, each step taken to better understand, diagnose, and treat these conditions brings us closer to a future where the hidden complexities of autoimmune illnesses are no longer intimidating mysteries but manageable conditions with clear paths to recovery.
In a time when every moment counts, and when the little details often hold the key to a patient’s survival, we must continue to invest in both our clinical expertise and our ability to connect on a human level. Only then can we ensure that the right diagnosis at the right time is followed by the right treatment—a formula that, as this case shows, can make all the difference.
Originally Post From https://www.cureus.com/articles/349053-friday-night-acute-kidney-injury-chest-infection-masking-antineutrophil-cytoplasmic-antibody-vasculitis
Read more about this topic at
Understanding the impact of delayed diagnosis and …
Autoimmune disorders: MedlinePlus Medical Encyclopedia