Examining the High-Cost Drug Funding Debate: An Opinion Editorial
State legislators across the nation are currently embroiled in a heated discussion regarding the use of alternative funding programs for prescription drug benefits. These programs are designed to help manage the steep costs of expensive medications. However, they come with their own set of tricky parts, tangled issues, and confusing bits that have both supporters and critics alike. This op-ed takes a closer look at alternative funding strategies, questions whether these methods are truly beneficial for patients, and assesses the broader implications for healthcare regulation.
Understanding Alternative Funding Programs and Their Purpose
Alternative funding programs (AFPs) have emerged as a response to the explosive costs associated with some specialty drugs. In an effort to keep premiums at bay, health plans and large plan administrators have increasingly resorted to these approaches. Rather than covering every expensive medication outright, some AFPs deliberately exclude coverage for a handful of very pricey drugs. Instead, they operate on the assumption that pharmaceutical manufacturers or charitable organizations will help cover the cost for those who critically need them.
The rationale behind this strategy is fairly straightforward: by shifting part of the financial responsibility, employers can avoid passing on unsustainable premium hikes to their employees. Yet, this approach is not without its twists and turns. Critics argue that while this method might work on paper, its application in real life is more daunting, with many patients navigating an overwhelming maze of alternative payment channels.
State Legislators Weigh In: Balancing Costs and Patient Needs
Recent discussions in state legislatures have brought this issue into sharp focus. For instance, in Utah, a prominent health plan administrator has been actively promoting the AFP strategy to employers. Republican state representative Jim Dunnigan explained that the use of alternative funding programs is seen as a reasonable tactic to mitigate skyrocketing drug costs. According to Dunnigan, the philosophy behind the AFPs is that not “millions of people out there are waiting to pay significantly higher insurance premiums.”
However, the legislative dialogue is far from one-sided. Lawmakers are also expressing concerns that these AFPs may leave some patients stranded without access to their necessary medications. The debate has evolved into a broader discussion on whether regulation of AFPs—rather than outright bans—could offer a balanced solution that protects patients while keeping costs manageable.
In one example, legislators from Illinois, such as Republican state representative Jeff Keicher, suggested that licensing and regulating these programs might be a more effective response. This idea brings forth a central question: How do we reconcile cost containment with the guarantee of patient access to life-saving drugs?
Patient Impacts: Navigating a Labyrinth of Financial Pathways
For many patients, especially those with chronic or life-threatening conditions, the implementation of alternative funding programs can seem like navigating a labyrinth of financial twists and turns. On one hand, the promise of lower insurance premiums is appealing, particularly to employers and cost-conscious policyholders. On the other hand, the idea of having to rely on pharmaceutical companies or charities to cover the cost of essential medications is a nerve-racking prospect.
Theresa Alban, the federal policy director at the Cystic Fibrosis Foundation, has raised red flags about the safety and reliability of some AFP providers. She noted that several providers have been advocating the importation of drugs under federal laws as a safe and cost-effective measure. Yet, in real-world scenarios, patients with cystic fibrosis have faced significant difficulties when attempting to import their medications. Alban’s comments underscore the many subtle details and fine shades of this issue that make it difficult for patients to have confidence in the AFP system.
Below is a bullet list summarizing some of the key benefits and potential pitfalls for patients when AFPs are implemented:
- Potential Benefits:
- Reduced premium costs for many policyholders
- Incentives for pharmaceutical manufacturers to lower prices
- Introduction of innovative pricing models in healthcare
- Potential Pitfalls:
- Risk of patients not receiving timely access to certain medications
- Over-reliance on charitable organizations and external funding sources
- Confusing administrative processes that can further complicate patient care
Industry Perspectives: Behind the Scenes of AFPs
From an industry standpoint, alternative funding programs are both a reaction to and a catalyst for change in the high-cost drug market. With pharmaceutical companies often setting exorbitant prices, AFPs have emerged as a strategy to curb the financial pressure on employers and insurers. Yet, the method remains loaded with issues.
Plan administrators tout AFPs as a cost-saving measure that can alleviate some of the economic pressure on large employers. For example, one large plan administrator in Utah has reportedly offered these programs as an option for businesses striving to balance high drug costs with the need to keep premiums affordable. The idea is that if manufacturers or charities can cover a significant share of the costs for the most expensive drugs, then employers may be able to maintain lower overall expenditures.
However, several industry insiders argue that while AFPs might appear to be a promising workaround, they often introduce more confusing bits and tangled issues. The unpredictable nature of relying on external funds can result in delays and administrative complications. Additionally, there is notable concern about the long-term sustainability of such programs, particularly if manufacturers or charity organizations do not consistently contribute their share.
Consider the table below which highlights an overview of the pros and cons from an industry viewpoint:
| Aspect | Pros | Cons |
|---|---|---|
| Cost Savings | Lower premiums for employers; potential cost sharing with manufacturers and charities | Uncertain funding sources may lead to inconsistency |
| Administrative Efficiency | Streamlined plans may reduce some administrative overhead | Complex application and processing procedures can create delays |
| Market Dynamics | Encourages competitive pricing among manufacturers | May lead to unintended gaps in patient care if not properly managed |
This table provides a snapshot of the key factors that industry stakeholders must consider when promoting or implementing AFPs. It becomes clear that while the alternative funding approach offers some attractive benefits, its many hidden complexities require careful management and, ideally, regulatory oversight.
Regulatory Considerations: Finding a Way Through the Maze
The debate over AFPs has brought regulatory considerations to the forefront of healthcare discussions. Many legislators are working through an intense series of discussions to figure a path that balances affordability with patient care. There is a growing consensus that the AFP model should not be abandoned outright but rather improved through better oversight and licensing.
For instance, proposals for licensing and regulating AFP providers aim to ensure that these programs are held to strict standards. Such regulation could address many of the hidden complexities—like inconsistent funding, confusing administrative procedures, and potential lapses in patient access—that currently plague the system. Legislators in some jurisdictions are advocating for a framework where AFP providers are required to meet rigorous performance benchmarks before they are allowed to operate.
Key proposals under discussion include:
- Establishing standardized guidelines for AFP participation
- Requiring formal audits and financial transparency from AFP providers
- Implementing patient feedback mechanisms to promptly address issues
- Integrating regulatory oversight with state and federal healthcare agencies
Each of these proposals is targeted at mitigating the risks associated with AFPs by ensuring that the programs do not inadvertently create additional hurdles for patients. By licensing providers and enforcing strict standards, regulators hope to tame the tangled issues that make alternative funding strategies feel so overwhelming.
Exploring the Alternative: Are There More Effective Solutions?
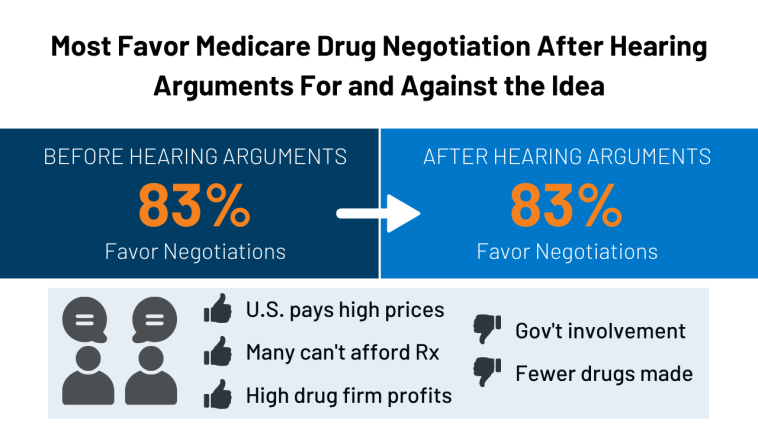
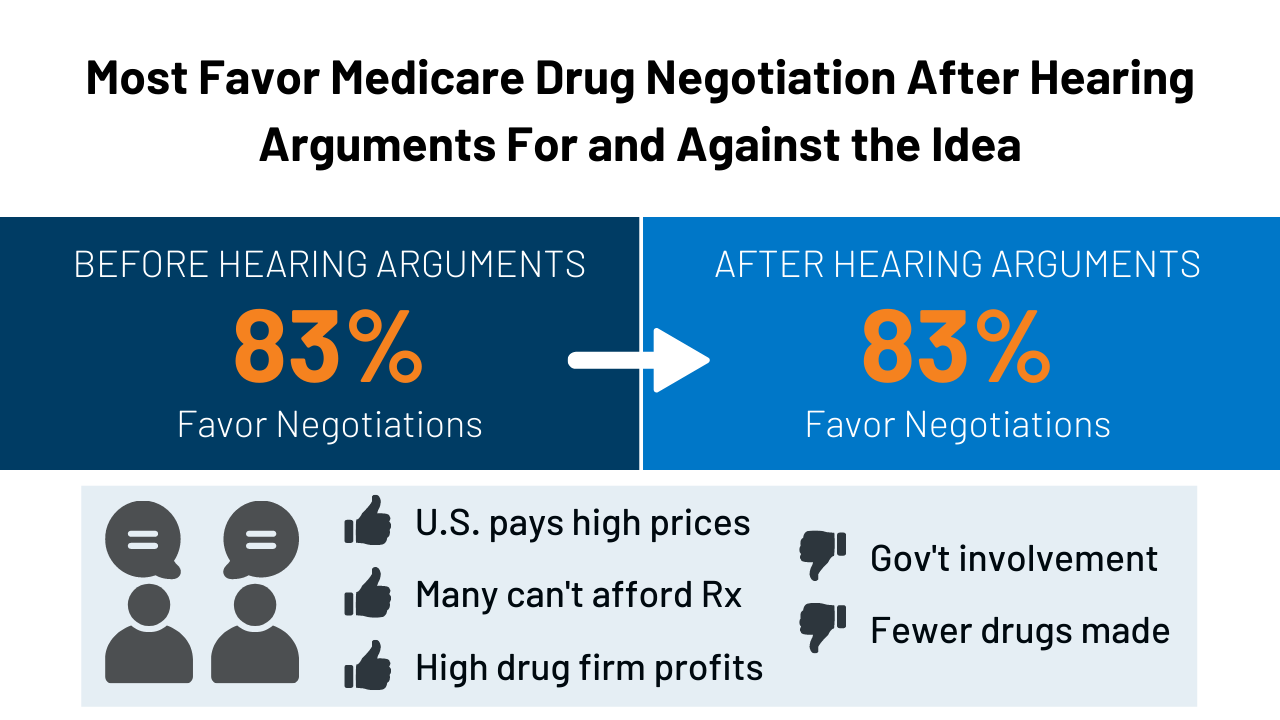
While AFPs represent one approach to dealing with skyrocketing drug costs, some critics argue that alternative solutions might be more effective in the long run. One such counterproposal involves more aggressive price negotiations directly with manufacturers. This strategy, which has been employed in other developed nations, seeks to directly address the root of the problem rather than symptoms introduced by complex funding mechanisms.
Other ideas include:
- Value-based pricing models that tie drug costs to patient outcomes
- Expanded government subsidies or rebates for high-cost medications
- Enhanced transparency initiatives to better understand the pricing mechanisms of drugs
Each of these proposals has its own set of twisted issues and challenging bits. For example, negotiating drug prices at scale often requires negotiating with powerful industry players—a process that can be both intimidating and nerve-racking for policymakers and healthcare providers alike.
Proponents of direct pricing negotiations argue that this method is more sustainable because it attacks the high cost issue at its source. Instead of relying on external funding, a more direct approach could eliminate the need for a complicated layer of alternative funding programs altogether. However, achieving such reforms is a long and winding road, full of both expected and unexpected hurdles.
Economic Impact and the Future of Healthcare Spending
Beyond its immediate effects on patient care, the use of AFPs has significant implications for the overall economy and the future of healthcare spending. As employers increasingly lean on these programs to cut costs, the broader market could experience shifts that impact everything from drug research and development investments to the way pharmaceutical companies price their products.
Critics contend that handing off expensive drugs to an alternative funding mechanism might inadvertently stifle innovation in the long run because manufacturers could lose the incentive to keep prices in check. This scenario could lead to a vicious cycle where drug prices continue to escalate despite efforts to manage them through AFPs. The interplay between cost control and encouraging innovation presents a series of confusing bits and subtle parts that policymakers must carefully weigh.
It may be useful to consider the financial impact of AFPs in the form of a breakdown:
| Impact Area | Potential Positive Outcome | Possible Negative Outcome |
|---|---|---|
| Employer Costs | Reduced premiums and lower financial liability | Risk of unexpected patient care costs if funding fails |
| Pharmaceutical Pricing | Pressure to negotiate lower prices | Possible reduction in R&D investments |
| Patient Access | Short-term relief from high premiums | Long-term access issues for patients requiring expensive drugs |
Such analyses underscore that any attempt to streamline high-cost drug funding must consider the far-reaching economic consequences. Cost control measures, while essential, should not compromise the broader ecosystem that supports medical innovation and patient care.
Policy Implications: Regulatory, Economic, and Ethical Considerations
The issue of alternative funding programs is not merely a financial debate—it also touches upon ethical considerations and the social responsibility of all parties involved. On one side, there is the strong need to keep healthcare affordable for both employers and patients. On the other, there lies the ethical imperative to ensure that no patient is left without access to critical, life-saving treatments.
Regulatory agencies are now confronted with a dilemma: Should they allow AFPs to proceed with minimal oversight, trusting that market forces will correct any imbalances over time? Or should they step in to regulate these programs more heavily, risking additional administrative burdens and potential delays in patient care? The answer, it seems, lies in finding a middle ground—a balanced regulatory framework that promotes transparency, accountability, and efficiency.
Some of the super important policy questions being raised include:
- What standards should AFP providers meet to ensure reliability?
- How can regulators work with industry stakeholders to create a robust oversight mechanism?
- Should there be a contingency plan in place in case AFPs fail to secure necessary funds?
- How do we protect patient access without squeezing the economic lifelines of employers?
Addressing these questions requires cooperation between state and federal regulators, employers, pharmaceutical companies, and patient advocacy groups. A coordinated strategy that listens to all stakeholders may be the best way to work through this tangled web of issues.
Comparing Alternative Funding to Other Cost-Containment Strategies
It is instructive to compare AFPs with other cost-containment strategies in healthcare. Traditional methods, such as direct price negotiation, government subsidies, and mandated rebates, have their own set of small distinctions and subtle details that set them apart from the AFP model.
Below is a brief comparison in the form of a bullet list:
-
Alternative Funding Programs:
- Emphasize shifting the funding burden away from employers
- Rely on external sources like charities and manufacturers
- Allow for lower premiums, but potentially at the expense of direct patient support
-
Direct Price Negotiation:
- Focuses on reducing the baseline cost of medications
- Works directly with manufacturers to set prices
- Offers a more transparent and controlled approach, though it may be harder to implement quickly
-
Government Subsidies:
- Provide direct financial support to lower drug costs
- Reduce the financial risk for patients
- Depend on political will and budget allocations that can shift with administrations
Each of these strategies has its own set of benefits and shortcomings, and the ideal solution may well involve a mix of approaches. By blending targeted regulation with innovative funding mechanisms, policymakers may be able to craft a system that not only controls drug costs but also ensures comprehensive patient care.
The Road Ahead: Charting a Course Through Regulatory Uncertainty
As the debate over alternative funding programs unfolds, the healthcare community at large finds itself at a crossroads. The path forward is laden with both promising opportunities and nerve-racking uncertainties. Healthcare providers, employers, legislators, and patients are each trying to figure a path through this maze of issues.
Future developments in this area will likely depend on several factors:
- Policy Revisions: The evolution of regulatory frameworks that can adapt to new funding models while protecting consumer rights.
- Market Dynamics: The willingness of pharmaceutical companies and charities to reliably shoulder part of the funding burden.
- Patient Advocacy: The degree to which patient groups can influence policy to ensure that cost savings do not come at the expense of vital healthcare access.
- Technological Innovations: The emergence of new data tools and analytics that can help regulators monitor AFP performance in real time.
To steer through these confusing bits and overlapping interests, it is imperative that all stakeholders remain committed to open dialogue and continuous improvement. While the AFP model is still in its infancy, experience and careful regulatory oversight could ultimately transform it into an essential tool for managing high drug costs.
Conclusion: Striking the Delicate Balance Between Cost and Care
In conclusion, the debate around alternative funding programs for high-cost drugs is emblematic of the larger struggles within modern healthcare. On one hand, there is a clear need to contain costs and protect employers from astronomical premium hikes. On the other, patients must not be left to navigate a maze of intimidating financial alternatives when they need critical medications the most.
Legislators, industry experts, and patient advocates must continue to take a closer look at both the fine points and the little details of AFPs, striving for a balanced approach that does not sacrifice access for affordability. In doing so, it is super important that a transparent, regulated, and accountable system is established—one that effectively addresses the tangled issues head on. Only by working together can all parties figure a path that meets the needs of today’s complex healthcare landscape.
As this debate continues to evolve, one thing remains clear: the future of high-cost drug funding hangs in the balance. Will alternative funding programs become a mainstay of cost control, or will they be supplanted by more direct and sustainable measures? The answer may ultimately depend on the willingness of regulators and policymakers to dive in, steer through the nerve-racking twists and turns, and ultimately craft a solution that is as compassionate as it is cost-effective.
In the end, the hope is that through well-designed regulations and calculated policy shifts, we can strike a delicate balance—one that keeps healthcare affordable for employers without compromising the essential care that patients depend on. It is a challenge that is loaded with issues, but one that must be taken on if we are to ensure the well-being of all those who rely on our healthcare system.
Originally Post From https://www.benefitspro.com/2025/11/17/state-legislators-debate-regulation-of-alternative-funding-programs-for-high-cost-drugs/
Read more about this topic at
State legislators debate regulation of ‘alternative funding …
Trump’s broadside against health insurers is a cautionary …