Opinion: Microultrasound Technology Revolutionizing Prostate Cancer Diagnosis
In the ever-evolving landscape of modern medicine, innovations that simplify tricky parts of diagnosis are always welcomed. The recent data emerging from a large-scale clinical trial has shone the spotlight on micro-ultrasound technology. This promising modality has quickly captured the attention of urologists and healthcare professionals worldwide. As a seasoned observer of both conventional and alternative medicine, I find that microultrasound offers an appealing blend of high-quality imaging with improved accessibility. In this op-ed, I will take a closer look at how this technology is reshaping the way we approach prostate cancer diagnosis, and why it may soon be the key alternative to the more traditional magnetic resonance imaging (MRI).
The study in focus, the OPTIMUM randomized clinical trial, compared the ExactVu micro-ultrasound platform with the standard MRI/conventional ultrasonography fusion-guided approach. With over 800 patients included from various international sites, the trial’s results have established that microultrasound-guided biopsy is noninferior to MRI guidance in detecting clinically significant prostate cancer. This breakthrough not only underscores the technical prowess of microultrasound but also highlights how innovations can bridge gaps in patient care by addressing both accessibility and cost concerns.
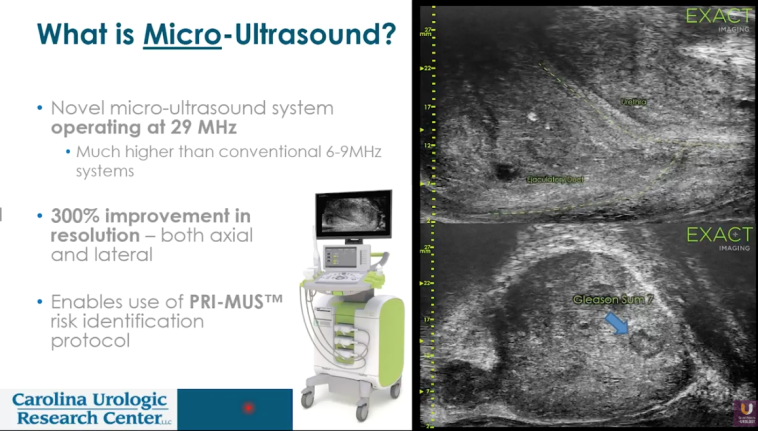
Micro-Ultrasound as a Game-Changer in Prostate Imaging
The advantages of employing microultrasound go beyond mere effectiveness in identifying clinically significant prostate cancer. The modality is designed to be used in an in-office setting, making it an appealing alternative to MRI-based assessments that often require scheduling delays and additional appointments. In practical terms, this means that patients can receive a diagnosis promptly and confidently, sidestepping the nerve-racking waiting periods that are common with traditional imaging techniques.
From a clinical perspective, the trial demonstrated similar detection rates between the microultrasound and MRI approaches, with rates hovering around the mid-40% mark for meaningful disease. This similarity in performance is significant because it paves the way for the technology to be implemented even in clinics where MRI machines are not readily available. In many rural or resource-limited areas, the lack of advanced imaging facilities has long posed a challenge for proper diagnosis. Microultrasound, with its portability and in-office application, promises to level the playing field for patients everywhere.
Improving Prostate Cancer Detection in Everyday Clinical Settings
A key strength of microultrasound is its ability to seamlessly integrate into everyday clinical routines. For many urologists, managing the twists and turns of prostate cancer diagnosis has been complicated by scheduling conflicts and the high costs associated with MRI scans. With microultrasound, these challenges begin to dissipate. The device is easy-to-use and does not require the extensive infrastructure that MRI demands.
In addition, the technology helps reduce not only the tangible barriers of cost and logistics but also the intangible barriers such as the intimidating nature of advanced imaging for some patients. Many individuals who are wary of undergoing a large, off-putting MRI scan might instead opt for a procedure that is less overwhelming and can be conducted in a more familiar, comfortable setting. This shift could lead to earlier intervention and better outcomes, particularly in populations that have historically had limited access to high-end diagnostic tools.
Cost-Effective and In-Office Approach: A Closer Look
Cost plays a significant role when choosing diagnostic modalities, both from the perspective of healthcare systems and patients. Microultrasound stands out for its cost-effectiveness. Traditional MRIs are not only expensive but also resource-intensive. Many clinics struggle with the high overhead required to purchase, maintain, and operate MRI equipment. Microultrasound, on the other hand, offers a more compact and affordable solution that can produce quality images without the need for elaborate setup.
Below is a table summarizing a few key comparisons between microultrasound and MRI-guided biopsy:
| Parameter | Microultrasound | MRI-Guided Biopsy |
|---|---|---|
| Cost | Relatively low | High overhead |
| Accessibility | In-office, immediate use | Often requires referral to specialized centers |
| Patient Convenience | Quick setup and familiar setting | Time-consuming and sometimes invasive |
| Diagnostic Accuracy | Noninferior to MRI in detecting clinically significant cancer | Considered the standard of care |
This breakdown helps illustrate that while MRIs have long been the stalwarts in prostate imaging, microultrasound has made a compelling argument for itself. By offering similar diagnostic performance combined with pragmatic benefits like cost reduction and easy accessibility, this tool is well-poised to make a real difference in everyday clinical settings.
Addressing the Intimidating Side of Advanced Diagnostics
The human aspect of undergoing any medical procedure cannot be understated. Many patients find the traditional diagnostic journey laden with confusing bits and intimidating procedures that create additional anxiety. With micro-ultrasound, clinicians are equipped with a tool that simplifies this process significantly. The procedure can be performed in an office without the nerve-racking delays associated with scheduling an MRI, making it a far more attractive option for patients who are already grappling with the fear of a cancer diagnosis.
The improved patient experience is a win-win situation. Not only do patients benefit from less stressful and more accessible diagnostic procedures, but healthcare providers also find success in establishing trust and delivering prompt care. A less overwhelming experience can encourage more patients to get screened early, potentially catching prostate cancer in its earlier, more treatable stages.
Enhancing Accuracy with Dual-Mode Imaging Techniques
One of the fascinating aspects of the OPTIMUM trial was the evaluation of a combined approach, where microultrasound was used alongside traditional MRI. This dual-mode imaging technique was shown to slightly improve the detection rate of clinically significant prostate cancer compared to using MRI fusion alone. Although the improvement may seem incremental at first glance, even subtle details can have a profound impact when it comes to life-altering diagnoses.
The combined method leverages the strengths of both imaging modalities. On one hand, MRI offers excellent soft tissue contrast, while microultrasound excels in real-time imaging and ease-of-use. The trial’s favorable outcomes not only validate the role of micro-ultrasound as a standalone diagnostic tool but also suggest that its integration with established imaging methods can lead to even better results. Some potential benefits of the combined approach include:
- Improved overall diagnostic accuracy by compensating for the fine points that each method might miss individually.
- Ability to confirm findings from one modality with another, thus reinforcing the confidence in clinical decision-making.
- Enhanced patient outcomes by potentially lowering the rate of false negative results, which is critical in cancer diagnosis.
Reducing Healthcare Disparities Through Innovative Technologies
Healthcare is riddled with tension when it comes to equity in access. In many parts of the world, advanced diagnostic tools like MRI are not easily available, leading to delays in diagnosis and treatment. Microultrasound technology has the potential to act as a great equalizer in this context. With its compact design and lower cost, clinics in resource-limited settings could adopt this technology more readily.
By offering a tool that is both affordable and effective, we can begin to address the pressing issue of healthcare disparities. The ability to perform in-office biopsies means that even patients in more remote or underserved communities can “find their way” to earlier, life-saving diagnosis and treatment. This is not just a win for technology—it’s a win for public health and social justice.
Integrating New Diagnostic Modalities into Routine Practice
The transition from established methods to newer techniques always comes with its own set of challenges. Many practitioners are accustomed to the reliable performance of MRI and the well-trodden paths of conventional ultrasonography. Changing practice patterns can seem overwhelming or off-putting at first, especially when the new technology brings with it its own little twists. However, the evidence from the OPTIMUM trial suggests that integrating microultrasound is not only feasible but also a boost to routine practice.
For clinicians, adopting this technology means steering through some of the puzzling bits associated with new devices. However, the overall benefits for both practitioners and patients far outweigh the nerve-racking initial period of adjustment. With the support of robust clinical data and the promise of improved patient outcomes, many are now eager to integrate microultrasound into their everyday workflows.
Real-World Implications for Prostate Cancer Management
In the real world, the adoption of emerging technology must be justified by demonstrable improvements in patient care. In the context of prostate cancer management, microultrasound has shown that it is a super important addition to the diagnostic toolkit. Its ability to confirm significant findings without necessitating a referral to expensive MRI facilities holds promising implications for better disease management.
Consider the following benefits for real-world practice:
- Time Efficiency: The in-office procedure cuts down waiting times and streamlines patient flow.
- Economic Advantages: Lower costs mean that more patients can be screened without stretching healthcare budgets to the limit.
- Improved Follow-Up: Faster diagnosis allows clinicians to “get around” delays in initiating treatment, which is critical for a cancer that can be aggressive if left unchecked.
- Patient Comfort: The less intimidating environment of a standard clinic can reduce the anxiety often associated with diagnostic procedures.
These factors combined can transform the journey from suspicion to diagnosis into one that is as smooth and reassuring as possible. For many patients who have spent years grappling with billboards of uncertainty and confusing bits of conflicting advice, such innovations are both refreshing and crucial.
Patient-Reported Outcomes: Weighing the Benefits Beyond the Numbers
While clinical metrics such as detection rates are critical, the overall experience of patients undergoing diagnostic tests must also be a key consideration. In the quest to improve prostate cancer diagnosis, it’s essential to not only focus on the detectable outcomes but also on how patients feel about the processes. Anecdotal evidence and early patient feedback suggest that microultrasound is less intimidating and more patient-friendly compared to conventional methods.
When we take a closer look at patient-reported outcomes, several themes emerge:
- Reduced Stress: Patients report feeling less overwhelmed by the familiarity and simplicity of the microultrasound procedure.
- Enhanced Communication: The real-time imaging enables clinicians to better explain findings on the spot, helping patients understand their condition without resorting to overly technical explanations.
- Faster Results: Immediate imaging leads to quicker decisions about subsequent interventions, which can reduce the waiting game that so often exacerbates patient anxiety.
These subtle details remind us that improvements in medicine are not measured solely in percentages or p-values but also in how we make the patient journey smoother. As professionals, it is important to manage our way through both the hard data and the little human twists that ultimately define patient care.
Lessons Learned: What This Means for the Future of Diagnostic Medicine
The introduction of microultrasound in prostate cancer diagnostics offers several key lessons for the broader medical community:
- Adaptability: New technologies often require us to figure a path through the confusing bits of change. Clinicians need to be willing to experiment with innovative techniques that may eventually become the new standard of care.
- Collaboration: The successful integration of microultrasound into clinical practice is a testament to the collaborative spirit between researchers, device manufacturers, and clinicians. Working together, they have managed the transition from conventional methods to something that shows remarkable promise.
- Patient-Centered Care: At the heart of every medical innovation is the desire to improve patient outcomes. Whether it’s through more efficient diagnosis or less intimidating care protocols, the ultimate goal remains undiminished: delivering quality care and easing the burden on the patient.
- Continuous Improvement: The study’s findings are only one step in what is likely to be a long journey of refinement and integration. As more data comes in and more clinics adopt micro-ultrasound, we can expect further innovations that address even the fine shades in the patient care experience.
These lessons are super important not only for urologists but for all who are engaged in the pursuit of better, more accessible healthcare solutions. The willingness to take a closer look at emerging technologies will undoubtedly pave the way for future breakthroughs that can transform other areas of diagnostic medicine as well.
Expert Perspectives: Clinicians Weigh In on Microultrasound
The opinions shared by leading clinicians, including professors of surgery and active researchers in prostate health, bring immense credibility to the microultrasound platform. Their advocacy for this approach is rooted in firsthand experience and a pragmatic view of the benefits it offers. Many experts highlight that the transition to micro-ultrasound is not just about matching existing standards—it’s about improving the entire diagnostic process.
It is fascinating to note that:
- Clinicians appreciate the device’s portability and ease-of-use, which enable them to work through the logistical challenges associated with large imaging machines.
- Patients benefit from a streamlined process that cuts down on waiting times and reduces the overall stress of diagnosis.
- Healthcare systems stand to gain from substantial cost savings while maintaining high standards of care.
Such expert perspectives underscore that while the transition period may be loaded with issues and a few nerve-racking adjustments, the end benefits are well worth the effort. As more specialists begin to look into the details of micro-ultrasound, the broader medical community can expect a gradual, yet steady, shift towards incorporating this technology into everyday practice.
Looking to the Horizon: Future Research and Developments
While the current data on micro-ultrasound is promising, there is still much to be uncovered as clinical research continues into this neat piece of technology. Ongoing studies will likely address additional, subtle parts of the technology’s performance, such as its role in early detection among high-risk populations and its integration with other diagnostic tools. Researchers are already planning long-term follow-up studies to assess the impacts of early treatment decisions driven by micro-ultrasound findings.
Areas ripe for future investigation include:
- Comparative Efficacy Studies: Direct comparisons between microultrasound and other emerging diagnostic imaging technologies to identify the ideal scenarios for each modality.
- Patient Satisfaction Metrics: Detailed analyses of patient-reported outcomes to further validate the benefits of “in-office” imaging, especially in underserved communities.
- Economic Impact Assessments: Evaluating how the transition to microultrasound influences long-term healthcare spending and resource allocation.
- Integration with Other Modalities: Investigating scenarios where microultrasound is used in tandem with molecular diagnostics and genomic testing to provide a more comprehensive view of the cancer landscape.
Such forward-thinking research endeavors are super important not only for validating microultrasound’s role in prostate cancer management but for inspiring further innovation across the diagnostic spectrum. As these studies get underway, the medical community will have opportunities to further refine and optimize the technology, ensuring that its benefits reach as wide an audience as possible.
Patient Empowerment and the Role of Early Diagnosis
One of the most significant ethical and practical questions in modern medicine is how to empower patients through early and accurate diagnosis. Prostate cancer, in particular, has been a thorny topic with many patients discouraged by the intimidating and often expensive diagnostic process. With the advent of micro-ultrasound, patients are presented with a tool that demystifies a complicated piece of the cancer diagnosis puzzle.
Early diagnosis is not just about catching a disease sooner—it is about saving lives. When patients are able to receive prompt, reliable diagnostic information in a familiar setting, they can make informed decisions about their treatment options without the added weight of a lengthy, overwhelming diagnostic journey. The psychological benefits of this approach are nearly as important as the medical benefits:
- Patients report feeling more in control of their treatment timeline.
- There is reduced anxiety associated with waiting for diagnostic results.
- A streamlined process can foster a stronger, trust-based relationship between patients and their healthcare providers.
In practical terms, these improvements mean that patients are more likely to follow up with necessary treatment and adhere to recommendations, thereby enhancing overall outcomes. When the journey from suspicion to diagnosis becomes less intimidating, patients are more apt to commit to regular screenings and early intervention, ensuring that the virus of uncertainty is met with clear, decisive care.
Challenges and the Road Ahead: Small Distinctions That Matter
Of course, no new technology comes without its set of challenges. While the promise of microultrasound is clear, the integration of any novel diagnostic tool into daily practice will involve a period of adjustment. There are still a few distracting bits that remain to be perfectly ironed out:
- Training Requirements: Clinicians must learn the fine points of operating the microultrasound device effectively. This involves understanding the hidden complexities behind image acquisition and interpretation.
- Standardization of Protocols: Establishing streamlined procedures for using microultrasound in diverse clinical settings is on the agenda. Getting around these procedural twists and ensuring consistency across different healthcare facilities will be key.
- Integration with Existing Systems: Many healthcare facilities have deeply ingrained workflows built around conventional imaging. Adapting these systems to include microultrasound will require thoughtful changes and a collaborative approach.
In addressing these challenges, the medical community must remain patient-focused and agile. The goal is to figure a path where the latest technology is not seen as a replacement for existing methods but as an enhancement that provides additional, critical insights. As clinicians and administrators work through these adjustments, the ultimate beneficiary will be the patient, who receives comprehensive, efficient, and less intimidating care.
Conclusion: A Step Toward a More Accessible Future in Prostate Cancer Care
In summary, the emergence of micro-ultrasound technology marks a significant advancement in the field of prostate cancer diagnosis. By offering an alternative that is not only cost-effective and accessible but also noninferior to the more established MRI techniques, microultrasound is poised to transform prostate care as we know it. Its ability to reduce the nerve-racking waiting times, lower the financial burden, and ease patient anxiety underscores its potential to be a must-have tool in routine urologic practice.
As healthcare professionals continue to work through the small distinctions and tricky parts of integrating this innovative technology into everyday practice, we can anticipate profound improvements in both diagnostic timelines and patient outcomes. The optimism surrounding microultrasound is well-founded—it represents a clear step toward finding our path in a world where every patient, regardless of location or resources, can benefit from essential diagnostic services.
The journey ahead will undoubtedly involve further research, training, and collaboration, but the early indicators are promising. From the rigorous clinical trial data to glowing experiences reported by both practitioners and patients, it is clear that the integration of micro-ultrasound into prostate cancer diagnostics is more than just a technological upgrade—it is a transformative step toward a more equitable and efficient healthcare system.
As we stand on the threshold of this new frontier in diagnostic medicine, it is worth celebrating the strides that have been made and embracing the opportunities that lie ahead. The convenience of in-office imaging, the affordability of the technique, and the potential for enhanced patient satisfaction are all signals of a future where prostate cancer care is more agile, inclusive, and effective.
The promise of microultrasound is a potent reminder that when innovation meets practicality, the entire healthcare ecosystem stands to benefit. It is an invitation for clinicians and researchers alike to take a closer look, dive in, and continue pushing the boundaries of what is possible in diagnostic medicine. By embracing these new methods, we are not just treating a disease—we are transforming the patient experience and setting a new standard for care.
In conclusion, while there will always be challenges to manage and small adjustments to sort out, the future of prostate cancer diagnosis looks decidedly brighter with micro-ultrasound leading the charge. Let us take this opportunity to celebrate innovation, support clinical advancements, and, most importantly, ensure that every patient has access to the best possible diagnosis and treatment options. By doing so, we can truly make a lasting impact on patient care and effectiveness in prostate cancer management.
Originally Post From https://www.urologytimes.com/view/microultrasonography-positioned-as-alternative-to-mri-for-image-guided-prostate-biopsy
Read more about this topic at
Optimising prostate biopsies and imaging for the future-a …
Soteria Medical: The revolutionary new way of taking Prostate …