Reassessing Glenohumeral Arthritis Treatment Options: An Opinion on Shoulder Surgery Choices
Glenohumeral arthritis has long been one of the trickiest parts of orthopedic surgery. For decades, patients and surgeons have faced a range of confusing bits when deciding between treatment options. One of the key debates in shoulder arthroplasty is whether to opt for total shoulder arthroplasty (TSA) or the ream and run (RnR) technique. In this editorial, we take a closer look at these two methods, comparing the tangled issues surrounding each procedure and exploring their respective pros and cons in patient management.
While both treatments aim to alleviate pain and restore mobility, they come with their own set of challenges and subtle differences. This opinion piece will poke around the fine points of the procedures, discuss the key factors influencing clinical outcomes, and examine patient selection criteria. We will also outline the nerve-racking rehabilitation demands of each while considering real-world considerations such as cost-effectiveness and patient adherence.
Understanding the Tricky Parts of Shoulder Arthroplasty
Shoulder arthroplasty, much like other joint replacement surgeries, involves several complicated pieces that can often seem overwhelming. Total shoulder arthroplasty, the more conventional treatment, typically replaces both the humeral head and the glenoid surface with prosthetic implants. This method has been widely used, particularly in elderly patients whose rotator cuff functions remain intact. Yet, in younger or more active patients, TSA has its share of nerve-racking pitfalls, including a risk of early glenoid component wear and the possibility of revision surgeries.
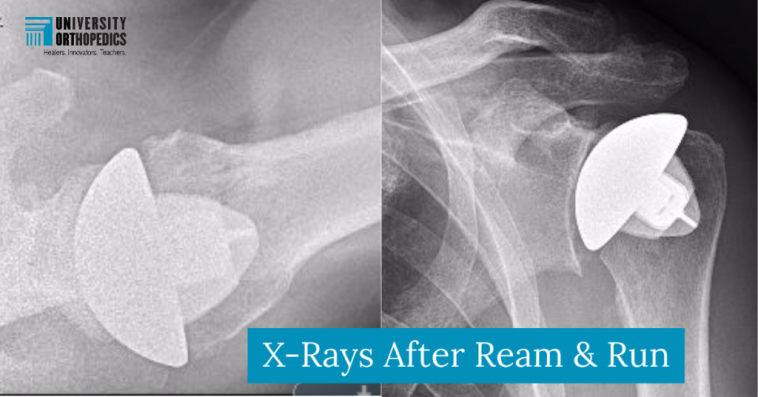
The ream and run procedure, an alternative that avoids glenoid component implantation, is seen as a promising option for select patients. By reshaping the glenoid bone rather than using a prosthetic, RnR focuses on triggering fibrocartilage regeneration that can eventually produce a durable, implant-free articulation. However, while its concept may seem conceptually straightforward, many surgeons find the intricacies of patient selection and postoperative rehabilitation to be quite tense.
Comparing Surgical Strategies: Total Shoulder Arthroplasty Versus Ream and Run
When it comes to managing glenohumeral arthritis, the decision between TSA and RnR ultimately boils down to balancing the pros and cons of each surgical strategy. On one side, TSA is known for its predictable early improvements in pain relief and functionality. On the other, RnR presents a viable treatment option that may appeal to younger, active individuals by eliminating the glenoid implant and its associated complications.
Despite improvements in patient outcomes for both methods, studies have revealed that RnR may be associated with a revision rate several times higher than that seen with TSA. Critics argue that the higher reoperation rate, coupled with the demanding rehabilitation process, makes the RnR pathway full of problems for many patients. However, supporters of the RnR procedure contend that, in the right hands and under proper conditions, it can offer comparable results to TSA with fewer long-term restrictions on activity.
Key Considerations Affecting Outcomes
Both TSA and RnR have shown significant improvements in key outcomes, including decreases in pain scores, better shoulder mobility, and enhanced overall function. However, the outcomes are intricately tied to several aspects:
- Patient Demographics: Younger patients, particularly those who are physically active, may benefit differently from one procedure versus the other. The typical TSA candidate is older, while RnR tends to be recommended for a younger, predominantly male demographic.
- Surgical Technique Variability: The RnR procedure itself is subject to technique variations—for example, differences in subscapularis management (using osteotomy, tenotomy-peel, or subperiosteal peel-back techniques) can affect the ultimate results.
- Rehabilitation Demands: Postoperative rehabilitation is another key issue. RnR imparts a nerve-racking level of commitment due to its reliance on immediate and aggressive post-surgery physical therapy to stimulate fibrocartilage formation, whereas TSA usually has a more “tried and tested” rehabilitation path.
- Revision and Reintervention Rates: Even though both procedures improve daily function significantly, the higher revision rate seen in RnR patients prompts some clinicians to prefer TSA for its lower likelihood of subsequent surgeries.
These subtle differences help shape treatment decisions, and understanding them is essential for both clinicians and patients. In many ways, deciding between TSA and RnR is all about figuring a path between early effectiveness and long-term durability.
Shoulder Function and Pain Relief: The Core Outcome Metrics
An examination into the outcomes of both procedures reveals that patient-reported measures—such as the Simple Shoulder Test (SST), American Shoulder and Elbow Surgeons (ASES) score, and Visual Analog Scale (VAS) for pain—improve significantly after surgery with either technique. The meta-analysis of available studies suggests that statistically, the improvements are comparable. That is, regardless of whether a patient undergoes TSA or RnR, both can experience dramatic improvements in shoulder function and pain reduction.
A closer look at these outcome measures indicates:
- The SST often shows a mean improvement that is nearly overlapping between the two methods.
- The ASES score, a key measure for athlete and daily-function evaluation, tends to improve similarly across both groups.
- VAS pain scores consistently decrease in both treatment cohorts, indicating that both procedures are effective at alleviating shoulder pain.
Thus, the clinical message is clear: Every patient deserves a tailored approach that considers both the short-term benefits and potential long-term issues, rather than a one-size-fits-all solution.
Rehabilitation: The Nerve-Racking Journey to Recovery
One of the most overwhelming aspects of shoulder arthroplasty—whether TSA or RnR—is the rehabilitation period that follows surgery. Rehabilitation after RnR, in particular, can feel like working through a maze, as it demands that patients are super important in their commitment to postoperative exercises. Immediate passive range-of-motion therapy is typically started from day zero, with the goal of molding the newly generated fibrocartilage in the reamed glenoid. The intensity of this regime often means that only patients who are mentally, emotionally, and physically primed for a long rehabilitation period should consider this option.
For many, the rehabilitation process can be intimidating, loaded with issues related to pain management, delayed recovery, and sometimes the need for later interventions. In comparing TSA with RnR, clinicians have noted that while TSA offers an arguably more straightforward rehabilitation, it is not completely free of challenges. Individuals who have undergone TSA might face restrictions in activity to protect the implanted components, making it equally important to set realistic expectations before surgery.
Ultimately, the decision about which procedure to choose should involve a frank discussion between the surgeon and patient about the rehabilitation journey ahead. Both paths require strong patient adherence and an understanding that recovery is both physically demanding and occasionally nerve-racking.
Patient Selection: Digging Into the Fine Points of Who Benefits Most
One of the fine points in making the right surgical decision is knowing which patient fits which treatment best. The studies comparing TSA and RnR suggest that the ideal candidate for the ream and run procedure might be a younger, active male with little history of depression or substance use. These patients tend to have a more optimistic outlook and are capable of investing in the long, intensive rehabilitation program that RnR demands.
Conversely, TSA might be a better match for older patients or those with comorbidities that could compromise the aggressive postoperative therapy that RnR requires. The decision is not just about age—it’s about a patient’s overall health, activity level, and commitment to rehabilitation. This tailored approach acknowledges that the decision-making process is full of tricky parts and that every patient’s scenario is as unique as their shoulder’s condition.
In summary, patient selection often involves assessing the following aspects:
- Age and Activity Level: Younger patients might benefit more from RnR, whereas older patients could find TSA more reliable.
- Psychological Readiness: A motivated patient who can commit to long-term rehabilitation is more likely to succeed with RnR.
- Medical History: Comorbidities or a history of substance use may tilt the scales in favor of TSA.
- Biomechanical Considerations: Specific patterns of glenoid wear and the degree of degeneration inform the recommended procedure.
This careful selection process underscores the importance of individualized treatment plans to overcome the many tangled issues that accompany glenohumeral arthritis management.
Surgical Technique Variability: Diving Into the Little Details
The nitty-gritty of surgical techniques can be full of problems that directly affect clinical outcomes. For TSA, the procedure is relatively standardized, yet it comes with its own twists and turns, including the risk of implant loosening and glenoid erosion over time. With the ream and run technique, differences in how the subscapularis muscle is managed can be particularly significant. Some surgeons opt for a subscapularis osteotomy, while others choose tenotomy-peel or a subperiosteal peel-back method. Such little details matter because they can shape how well the shoulder heals—and how quickly it regains function.
Even though studies show comparable functional outcomes between TSA and RnR, these subtle differences in surgical technique can have practical implications. For example:
| Surgical Technique | Advantages | Potential Challenges |
|---|---|---|
| Total Shoulder Arthroplasty (TSA) |
|
|
| Ream and Run (RnR) |
|
|
This table highlights some of the tricky and often nerve-racking decisions surgeons have to make each day. It is a reminder that the success of any procedure depends not just on the surgical act but also on precise, well-executed technique and careful patient management.
Revisiting Outcomes: What Do the Numbers Tell Us?
A careful look at the data from various comparative studies reveals that both TSA and RnR lead to significant improvements in shoulder function. Measures such as improvements in the Simple Shoulder Test score, ASES score, range of motion in active forward elevation, and external rotation have been observed in both cohorts. In addition, there is a substantial reduction in VAS pain scores after surgery.
Even though statistical differences between the two procedures are generally not significant, some fine shades in the data underscore essential considerations. For instance, while TSA may offer slightly better gains in forward elevation, RnR provides a comparable level of pain relief and functional improvement. These numbers are critical when discussing the potential benefits and risks of each procedure with patients.
To summarize some of the outcome metrics:
- SST Improvements: Both procedures show mean improvements of around 4.5–5 points.
- ASES Score Gains: Improvements are in the vicinity of 40 points for both techniques.
- Range of Motion Advances: Forward elevation and external rotation increase significantly, with differences between the two procedures being subtle.
- VAS Pain Reduction: Both procedures achieve a notable decrease in pain intensity postoperatively.
These numbers lend support to the idea that surgical choice should hinge on patient-specific factors rather than a blanket assumption that one technique is superior to the other. In today’s practice, it is key to blend statistical evidence with personal patient circumstances—a concept that remains super important in decision-making.
Evaluating Long-Term Sustainability and Revision Rates
One cannot ignore the ongoing debate surrounding the long-term durability of these shoulder arthroplasty procedures. TSA has stood the test of time in many clinical settings, providing reliable results over years. However, limitations such as implant wear, especially on the glenoid component, may necessitate revision surgeries down the line. For the ream and run method, higher revision rates have been noted in some studies; this can be especially intimidating for patients who are young and highly active.
It is important to dig into the literature and recognize that revision surgery isn’t just about a repeat operation—it is about subjecting the patient to additional recovery time, potential complications, and extra financial burdens.
Here are some of the challenges associated with long-term outcomes:
- TSA Risks:
- Considerable glenoid wear over time
- Possible need for revision due to implant loosening
- RnR Risks:
- Higher short-term revision rates in certain demographics
- Strict rehabilitation protocols that can influence long-term efficacy
In clinical practice, these long-term factors must be carefully weighed. Surgeons and patients need to figure a path that not only considers the early benefits but also the possible extended challenges. This involves taking a closer look at each patient’s lifestyle, surgical history, and future expectations.
Cost-Effectiveness and Real-World Considerations
The financial aspect of shoulder arthroplasty is another piece of the puzzle that is often on the edge of discussions in clinical settings. The cost-effectiveness of TSA versus RnR is a subject that continues to be debated among healthcare administrators and clinicians alike. While both types of shoulder surgery are resource-intensive, TSA might generate higher long-term costs through revision surgeries and extended postoperative care for implant preservation.
RnR, by potentially reducing complications associated with prosthetic components, might offer an attractive cost-saving alternative in the short term. Nonetheless, its higher revision rates observed in some studies can offset these savings, casting a slightly ambiguous picture regarding its economic benefits.
Some practical bullets to consider in evaluating cost-effectiveness include:
- Surgical Costs: Direct costs of the implant in TSA versus the implant-free concept of RnR.
- Rehabilitation Expenses: Intensive and lengthy rehabilitation may incur higher costs in RnR.
- Revision Surgery: Higher revision rates mean potential extra costs, regardless of the initial procedure.
- Indirect Costs: Work absence, reduced productivity, and quality-of-life impacts should be factored into any analysis.
In many respects, the choice between TSA and RnR becomes not just a matter of surgical approach but also a cost-benefit analysis that involves real-world factors. Clinicians must steer through these financial considerations while keeping patient care at the forefront of their decisions.
Patient Perspectives: Balancing Expectations and Reality
It is super important to consider how patients view the trade-offs between TSA and RnR. For many individuals, the decision is hampered by the overwhelming amount of information and the nerve-racking nature of long-term commitment to rehabilitation. Patients often inquire about the realistic outcomes and the degree of commitment required to achieve optimal results.
From the patient’s perspective, key concerns include:
- Ability to Return to Normal Activities: Will the procedure allow them to resume sports or daily tasks without limitations?
- Risk of Future Surgery: Understanding the likelihood of needing a revision procedure is a prominent worry.
- Recovery Timeline: Clear communication regarding the length and intensity of rehabilitation is crucial.
- Overall Satisfaction: Beyond the clinical data, how satisfied will they feel with their improved quality of life after surgery?
By getting into these topics, clinicians can provide a balanced picture using plain language that addresses the small distinctions between the two procedures. Ultimately, ensuring that patients have realistic expectations is as essential as the surgical procedure itself.
Expert Opinions and Current Trends in Shoulder Arthroplasty
Across the globe, orthopedic experts continue to debate which procedure might be better suited to particular patients. While the evidence suggests that both TSA and RnR offer significant improvements in functionality and pain relief, the choice often comes down to the individual clinical scenario and the surgeon’s experience. Some experts note that the ream and run procedure can be a game-changer for younger patients who place higher demands on their shoulders, provided the patient is committed to the rigorous rehabilitation required after surgery.
At the same time, total shoulder arthroplasty remains a trusted option for conserving joint function in cases where the rotator cuff is intact, and the patient’s activity level is moderate. As clinical techniques evolve and surgeon expertise grows, we are likely to see further refinements in both approaches. The ongoing debate, therefore, is not about which technique is inherently better, but rather about how to best match the procedure with the individual patient’s anatomical and lifestyle needs.
Recommendations for Surgeons and Clinicians
Looking at the current evidence and expert opinion, here are some super important recommendations for those managing patients with glenohumeral arthritis:
- Individualized Care: Every patient is unique, and the choice of procedure should be centered on their specific needs, health profile, and expectations.
- Thorough Preoperative Evaluation: Patients should be evaluated not only on physical parameters but also on psychological readiness and commitment to a lengthy rehabilitation regimen if RnR is considered.
- Clear Communication: Surgeons must explain the twists and turns of each treatment option in simple language, ensuring patients understand the potential benefits and limitations.
- Interdisciplinary Approach: Involving physical therapists, pain management experts, and even financial counselors can help patients navigate the whole process.
- Long-Term Follow-Up: Rigorous, long-term follow-up is essential to monitor the durability of the chosen procedure and to catch early signs of any complications.
These recommendations highlight the need for a holistic approach that goes beyond the operating room and addresses the tricky parts of patient care in a comprehensive manner.
Future Directions and Research Needs
Despite the wealth of data available, several subtle parts of this debate remain unresolved, inviting further research. Future studies should consider:
- Larger Multi-Center Comparisons: Current studies largely stem from high-volume academic centers, leaving a gap in our understanding of how these procedures perform in more diverse clinical settings.
- Long-Term Outcome Data: With maximum follow-up periods still under five years in many studies, the long-term durability of the RnR procedure, in particular, needs further exploration.
- Cost-Effectiveness Analyses: Including both direct and indirect costs could offer deeper insight into which procedure offers better value over time in different patient populations.
- Subgroup Analyses by Technique: Given the variation in subscapularis management during RnR, analyzing outcomes based on different surgical techniques might help refine patient selection criteria.
By taking a closer look at these areas, future research can help figure a path toward more personalized, effective treatments. It is clear that both procedures have their place, but refining the criteria for patient selection and understanding long-term outcomes will be key to improving overall shoulder arthroplasty care.
Final Thoughts: Balancing Benefits, Risks, and Patient Expectations
As we wrap up this discussion, the message is clear: both total shoulder arthroplasty and the ream and run technique offer substantial benefits, yet each comes with its own delicate twists and turns. The choice between TSA and RnR is filled with complicated pieces—from surgical technique variability and rehabilitation demands to patient-specific factors such as age, activity level, and psychological readiness.
Clinicians must therefore work closely with their patients to steer through the maze of options by weighing the pros and cons in a balanced, informed manner. It is essential that patients understand both the immediate benefits—as seen in improved pain scores and shoulder mobility—as well as the potential long-term implications, such as the risk of revision surgeries and the demand for relentless rehabilitation.
In the end, the goal is not to declare one procedure as definitively superior to the other, but to offer a tailored approach that takes into account the small distinctions, tricky parts, and individual needs of each patient. This patient-centered approach remains the key to ensuring optimal outcomes and overall satisfaction in managing glenohumeral arthritis.
By embracing both the established path of total shoulder arthroplasty and the promising, yet challenging, ream and run technique, healthcare providers can offer a spectrum of options that are super important for addressing the wide-ranging needs of patients. The ongoing evolution in surgical techniques and postoperative care will continue to shape the future of shoulder arthroplasty, providing hope for improved long-term outcomes and better quality of life for those suffering from glenohumeral arthritis.
Summary of Key Points
To summarize this discussion in a clear, organized manner, consider the following bullet points:
- Both TSA and RnR are effective in reducing pain and enhancing shoulder function.
- Patient selection is critical—factors such as age, activity level, and psychological readiness must be considered.
- The RnR procedure, while promising for younger and active individuals, comes with a higher revision rate and demanding rehabilitation protocol.
- TSA, though standardized and reliable for many, may carry long-term risks such as implant wear and glenoid component loosening.
- Cost-effectiveness and long-term patient satisfaction are important factors that require additional research and multi-center data.
- Clear communication and an interdisciplinary approach can help patients steer through these nerve-racking decisions.
These considerations form the bedrock of balanced clinical decision-making in the management of shoulder arthritis, ensuring that both patients and physicians are well-equipped to make informed choices.
Conclusion: Empowering Patients Through Informed Decision-Making
The choice between total shoulder arthroplasty and the ream and run procedure is much more than a technical decision—it is a nuanced, highly personalized journey. As this opinion editorial has outlined, the evidence suggests that both methods significantly improve shoulder function and reduce pain in patients with glenohumeral arthritis. However, the decision should be guided by an in-depth discussion of each option’s benefits and limitations, combined with a frank assessment of the patient’s ability to engage in intense rehabilitation and manage the longer-term demands of their chosen treatment.
Healthcare providers need to continue working through these issues with empathy and clarity—ensuring that patients not only receive the most appropriate treatment but also feel empowered by understanding every twist and turn of their surgical journey. As technological advances and clinical research continue to advance our understanding, the focus must remain on individualized care that respects both the art and science of shoulder arthroplasty.
In conclusion, whether you decide on TSA or RnR, the most important takeaway is that comprehensive patient evaluation and clear, compassionate communication will always be at the heart of successful treatment planning. By embracing innovation and continuing to assess long-term outcomes, the field can move toward even more effective and personalized solutions for shoulder arthritis care.
Originally Post From https://www.cureus.com/articles/339746-ream-and-run-hemiarthroplasty-versus-total-shoulder-arthroplasty-a-comparison-of-shoulder-treatments-for-glenohumeral-arthritis
Read more about this topic at
Comparison between Anatomic Total Shoulder …
Comparison between Anatomic Total Shoulder …