Herbal Remedies in Functional Gastrointestinal Disorders: An Opinion Editorial
The landscape of functional gastrointestinal disorders is full of tricky parts and tangled issues that challenge both patients and clinicians alike. Functional dyspepsia, constipation, and other motility disorders are common complaints that often leave patients feeling overwhelmed by the scary side effects of synthetic medications. In recent years, herbal remedies have emerged as a promising alternative that many experts find both natural and effective. This op‐ed examines a recent preclinical study comparing two herbal formulas designed to improve gastrointestinal function and modulate gut microbiota in a rat model of loperamide-induced dyspepsia. We will take a closer look at the study’s design, discuss the hidden complexities of herbal treatment strategies, and explore what these findings might mean for future clinical applications.
Understanding the Challenges in Gastrointestinal Health
Gastrointestinal disorders often present with confusing bits and complicated pieces. Many patients experience symptoms such as poor gastric motility, chronic constipation, and persistent abdominal discomfort. Given the nerve-racking array of available synthetic drugs, professionals are increasingly interested in alternative approaches rooted in traditional practices. These herbal formulas—developed and used for centuries in East Asia—are gaining traction because they promise fewer side effects and a more natural restoration of gut health.
Traditional herbal treatments target several axes: improvement of gut motility, restoration of the mucosal barrier, and rebalancing of gut microbiota composition. This multifactorial approach may offer a rational alternative to drugs that often come with their own set of side effects and dependency risks. However, the fine points of herbal interventions require extensive study to understand the small distinctions in their effects on various gastrointestinal parameters.
Comparative Evaluation of Two Herbal Formulas
Study Overview and Rationale
A recent experimental study used a well-established rat model of dyspepsia—created by administering loperamide—to evaluate the therapeutic potential of two herbal formulas. The formulas reviewed in the study are Shihosogan-tang (SST) and Yijung-tang (YJT). The research team compared these herbal treatments to mosapride, a synthetic prokinetic agent. The aim was to understand how each formula affects key parameters related to gastrointestinal (GI) function, such as intestinal length, transit time, mucosal integrity, and gene expression associated with hormones, tight junction proteins, and inflammatory markers.
Methodology in a Nutshell
The study used Sprague–Dawley rats, which were injected with loperamide to induce dyspepsia. The experimental design involved daily assessments of body mass, food intake, and fecal water content, as well as the measurement of serum ghrelin levels—a hormone known to regulate appetite and GI motility. Additionally, the investigators carried out histopathological analyses of intestinal tissue and evaluated gene expression related to intestinal permeability and motility. Fecal 16S rRNA gene sequencing was employed to determine changes in the gut microbiota, highlighting the effects of herbal formulas on microbial diversity.
Key Findings: A Tale of Two Formulas
The study produced a range of findings that illuminate the hidden twists and turns in herbal treatment of GI disorders:
- Intestinal Structure and Function: SST was effective in improving intestinal length and accelerating GI transit, as shown by the restoration of intestinal motility impaired by loperamide. YJT, on the other hand, excelled at enhancing the structure of the ileum by increasing villus length and muscular thickness.
- Hormone Regulation: SST was uniquely potent at restoring ghrelin levels decreased by loperamide, which has implications for gastric motility. YJT did not significantly affect ghrelin, suggesting that its primary benefits may lie elsewhere.
- Gene Expression Modulation: Both formulas influenced the expression of genes responsible for maintaining the intestinal barrier (such as ZO-1) and modulated inflammatory mediators like interleukin-6. However, SST’s effects on neurohumoral substances like bombesin appeared to be more pronounced, whereas YJT tended to support enteroprotection through improved intestinal structure.
- Gut Microbiota Alteration: Interestingly, while neither formula altered the overall species count (α-diversity), they produced significant shifts in the community composition (β-diversity) compared to loperamide alone. For example, changes in the relative abundance of Cyanobacteria, Firmicutes, and various genera were observed, indicating that herbal formulas can reshape the gut microbial ecosystem in subtle ways.
Overall, SST appears better suited for boosting GI motility, especially in scenarios where delayed gastric emptying and poor appetite are prominent. YJT, by contrast, shows promise for individuals with mild constipation and inflammation due to its stronger enteroprotective effects.
Herbal Formulas and Gastrointestinal Motility: The Hidden Twists and Turns
Intestinal Hormone Dynamics and Motility
One of the most fascinating aspects of the study is the impact of these herbal treatments on gut hormones. Ghrelin, the key hormone that energizes gastric motility, was significantly restored by SST. This might suggest that SST can help revive the nerve-rackingly sluggish gastrointestinal tract by countering the loperamide-induced deficiency in ghrelin. In contrast, YJT’s lack of influence on ghrelin points to different mechanisms at play, such as direct protection of the gut lining and modification of gene expression linked to water absorption.
The modulation of neuropeptides like bombesin and motilin further emphasizes how herbal formulas could favorably impact the fine points of GI tract regulation. The study found that bombesin expression was significantly enhanced with SST treatment, a finding that underscores its potential to improve motility by influencing the neurotransmitter network involved in smooth muscle contraction.
A Closer Look at the Role of Tight Junction Proteins
Maintaining the structural integrity of the intestinal barrier is essential for preventing infections and inflammation. The study revealed that YJT upregulated zonula occludens-1 (ZO-1), a protein crucial for the tight junction assembly between intestinal cells. This suggests that YJT may be particularly effective at reinforcing the defenses of the gut lining against the damaging effects that intoxicated motility and inflammation can cause.
Furthermore, neither herb showed significant changes in claudin-1 expression, but there was an observable reduction in water absorption regulators such as aquaporin-3 (AQP3) with SST treatment. Such subtle differences reflect the small distinctions between both formulas and illustrate that despite their seemingly similar herbal origins, their mechanisms are loaded with distinct issues that can lead to different clinical outcomes.
Gut Microbiota: The Microbial Puzzle and Herbal Influence
Understanding Microbiota Dynamics
The role of the gut microbiota in shaping gastrointestinal health is a topic filled with tricky parts and tangled issues. The beneficial effects of herbal formulas extend beyond hormonal regulation and tissue protection; they also include modifications to the gut microbial community. Although the overall microbial richness (as measured by the Chao1 index) remained stable across groups, the diversity of the microbiota (illustrated by the Shannon index) was noticeably enhanced in the YJT group.
This suggests that while the absolute numbers of different bacteria did not change, their evenness and relative balance did improve with YJT. The outcome is a more complex and potentially resilient microbial system that might play a protective role against the stressors associated with dyspepsia.
Specific Microbial Changes and Their Implications
An intriguing finding was the alteration of key microbial taxa following herbal treatments. SST was found to increase the relative abundance of Cyanobacteria and decrease Firmicutes compared to loperamide alone. These shifts could influence intestinal metabolism in ways that help restore motility and balance water absorption. Conversely, both formulas affected the levels of genera such as Alistipes, Allobaculum, Rhodospirillales, and Rikenellaceae_RC9, returning them to levels observed in normal animals.
The study even presented a heatmap correlation analysis, suggesting potential links between specific microbial shifts and changes in gene expression related to GI motility and inflammation. For example, increases in Blautia and Gastranaerophilales were uniquely associated with SST treatment. This table below helps summarize some of the microbial changes observed:
| Herbal Formula | Microbial Shift | Potential Impact |
|---|---|---|
| SST | ↑ Cyanobacteria, ↓ Firmicutes | May enhance intestinal metabolism and motility |
| YJT | ↑ Shannon diversity index | Improved microbial balance and resilience |
These findings demonstrate the potential for herbal formulas, by modifying the gut microbiota, to influence not only local intestinal processes but perhaps also systemic health through the gut-brain axis. The connections between microbial community alterations and the regulation of receptors such as TLR2 and TLR4 further emphasize the multifaceted roles these tiny organisms may play in gastrointestinal function.
Clinical Implications and the Road Ahead
Herbal Medicine as an Alternative Strategy
There is a growing sentiment among healthcare professionals that a re-examination of traditional herbal medicine is warranted. This study’s findings provide key insights into how herbal formulas like SST and YJT might be incorporated into therapeutic protocols for GI disorders. In cases where patients suffer from delayed gastric emptying, poor appetite, or stress-related dyspepsia, SST—with its aptitude for boosting ghrelin and improving motility—might serve as a promising option.
For other cases, especially where there is a significant degree of mucosal damage or inflammation, YJT’s enteroprotective effects suggest that it could help repair the intestinal lining. This direct targeting of the gut barrier function, as evidenced by upregulation of ZO-1 and improved histological markers, may cater to patients with mild constipation symptoms linked to inflammation. The potential to use such herbal approaches to avoid the off-putting side effects associated with many conventional drugs is super important for patients seeking natural alternatives.
Integrating Herbal Solutions into Modern Practice
Given that pharmaceutical treatments for GI disorders can sometimes be overwhelming and even intimidating, there is a definite need for complementary and alternative medicine options. Traditional herbal medicine brings several advantages, including natural sourcing, long-term historical usage, and the potential for fewer side effects. However, excepting the undeniable merits of these compounds, clinicians must also consider the nerve-racking fine points involved in interpreting experimental data and translating these findings into clinical practice.
Integrating herbal medicine into conventional therapy regimens will require:
- Robust Clinical Trials: While animal studies provide significant insight into the mechanisms at work, human clinical trials will be critical in verifying the efficacy and safety of herbal formulas.
- Standardization of Herbal Preparations: One of the challenges in using herbal medicine is ensuring that the formulations are consistent in terms of active ingredients. Advances in techniques such as high-performance liquid chromatography (HPLC) help standardize extracts like those used in SST and YJT.
- Personalized Healthcare: Gastrointestinal disorders manifest differently in each patient. An individualized approach that factors in the patient’s unique gut microbiome and specific GI motility issues will be crucial in deciding whether an herbal approach may be beneficial.
- Patient Education: Patients must be made aware of both the potential benefits and the twisting complexities of herbal treatments. Educating patients about possible interactions, dosing regimens, and the expected timeline for improvement is key to ensuring adherence and positive outcomes.
Barriers to Widespread Adoption
Despite the promise of herbal medicines, several hurdles remain before they can become a mainstay of gastrointestinal treatment. Some of these nerve-racking issues include:
- Regulatory Concerns: Herbal formulations often occupy a grey area in terms of regulation. Establishing universally accepted guidelines for production and clinical use is essential.
- Research Gaps: While preclinical studies are encouraging, there remains a need for long-term studies that assess safety, efficacy, and the potential for interactions with other medications.
- Variable Patient Responses: Individual differences in gut microbiota and genetic predispositions mean that the same herbal formula may not work uniformly for every patient. Further research into these small differences is loaded with issues but is necessary for personalized medicine.
Practical Considerations for Herbal Interventions
Dosage and Administration
One of the critical aspects for clinicians is determining the optimal dosage of herbal extracts. In the animal study under discussion, the authors used carefully calculated equivalent doses based on human clinical usage. For SST, the established dose was 1.4 g/kg/day, while YJT was administered at 2 g/kg/day. A successful transition from animal models to human application will require extensive dose-finding studies, taking into account factors such as bioavailability, metabolism, and potential herb–drug interactions.
It is also important to note that the method of extraction matters. Both herbal formulas in the study were prepared from herbs extracted in 30% ethanol, followed by freeze-drying. Consistency in extraction and preparation processes can ensure that patients receive a standardized and repeatable dose every time.
Monitoring Outcomes
In order to truly appreciate the effects of herbal treatments in clinical practice, healthcare providers should consider monitoring several key parameters:
- Gastrointestinal Transit Time: Non-invasive imaging or transit studies can help assess improvements in gut motility.
- Serum Hormone Levels: Monitoring hormones such as ghrelin may provide insights into the therapy’s impact on appetite and motility.
- Histopathological Markers: In cases of severe dyspepsia or inflammatory disorders, endoscopic biopsies could help gauge improvements in mucosal integrity.
- Microbiota Analysis: Advanced sequencing methods can track the subtle shifts in gut microbial composition that correlate with clinical improvements.
Such a multi-pronged approach will help identify which patients may be ideal candidates for herbal therapy and allow for nuanced adjustments if necessary.
The Role of Gut Microbiota in Modulating Response to Herbal Therapies
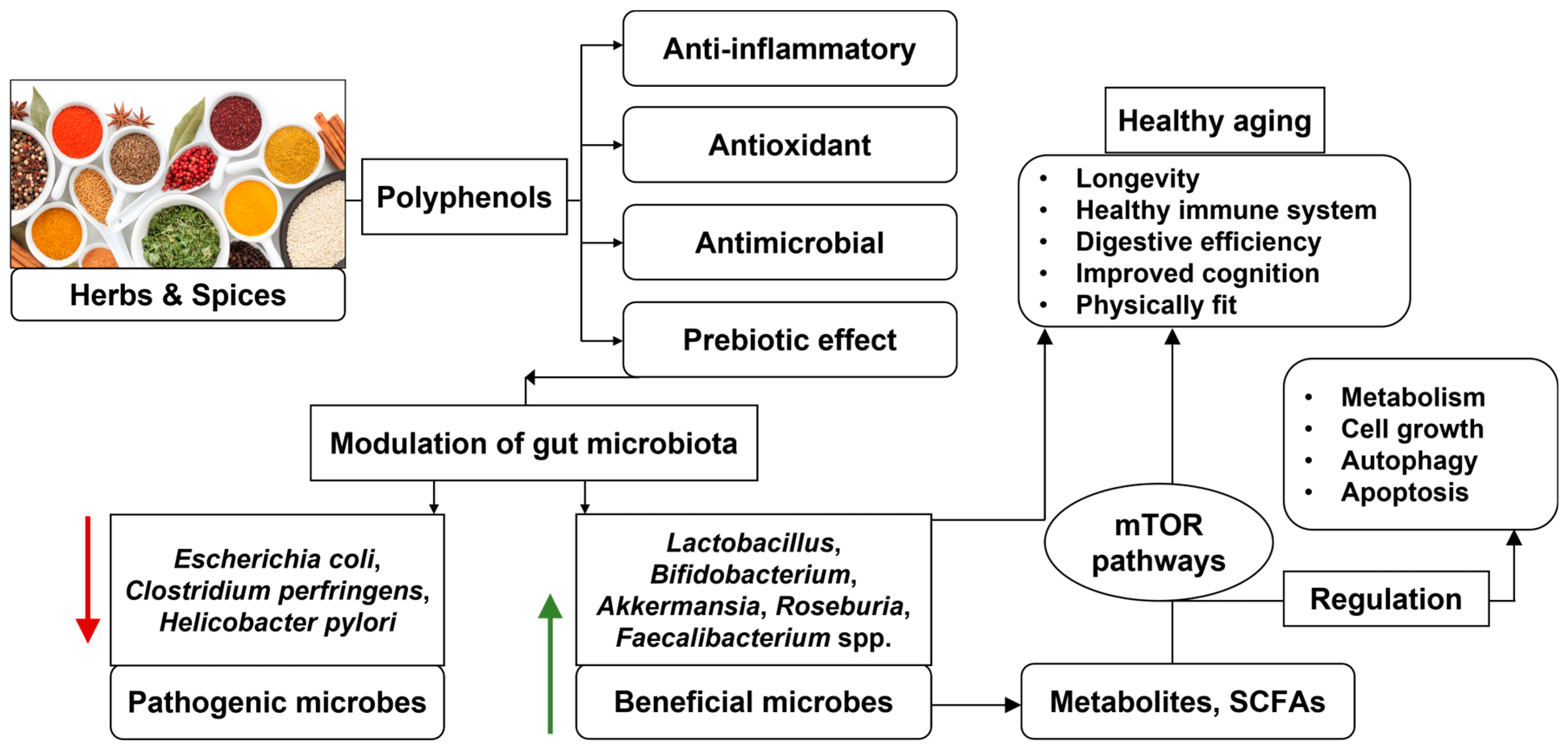
Interplay Between Microbes and Herbal Compounds
Recent advances in our understanding of the gut microbiota have unveiled how these microscopic organisms influence almost every aspect of health—including the processing of herbal compounds. The study discussed earlier points out that while SST and YJT did not affect the number of bacteria (α-diversity), they did alter the overall structure (β-diversity) in ways that likely affect gastrointestinal function. Such alterations suggest that the combination of herbal formulas and the patient’s resident gut microbiota can synergize to improve outcomes.
The following bullet list highlights some potential mechanisms:
- Herb Metabolism: Gut bacteria are capable of converting herbal constituents into bioactive metabolites that may then influence intestinal motility and inflammation.
- Immune Regulation: Changes in microbial composition can affect immune system balance, potentially reducing the inflammatory responses in the gut.
- Enhancement of Barrier Function: A balanced microbial ecosystem collaborates with herbal compounds to strengthen the gut’s mucosal barrier, thereby improving overall gut health.
Personalized Gut Microbiota Management
Clinicians aiming to harness the benefits of herbal remedies in gastrointestinal disorders need to appreciate the individual differences in gut microbiota. The study’s detailed correlation analysis between microbial shifts and changes in gene expression serves as a reminder that the impacts of herbal medicines are nuanced and patient-specific. In this context, personalized medicine—where treatments are tailored based on an individual’s microbial fingerprint—may represent the way of the future.
In summary, integrating gut microbiota analysis into treatment planning could help solve the tangled issues of variable responses to herbal therapy. By combining herbal therapy with prebiotic or probiotic administration, it might be possible to boost the efficacy of these treatments even further.
Looking Toward the Future: Research and Application
Opportunities for Further Investigation
The study comparing SST and YJT provides a solid starting point for understanding the distinct roles herbal formulas can play in managing gastrointestinal disorders. However, the research remains on the short-term side, and the long-term effects of these herbal treatments remain to be fully elucidated. Several key questions need to be answered in future studies:
- How do the active compounds in each herbal formula interact with the human hormonal system over time?
- What are the long-term safety implications of using these herbal remedies in patients with chronic GI conditions?
- Can a combination of herbal treatments and modern microbiota-targeting therapies provide superior results?
- How will personalized medicine approaches further optimize the use of herbal formulas based on individual genetics and microbiota profiles?
Addressing these tricky parts through rigorous clinical trials and multidisciplinary research initiatives is essential for integrating these herbal approaches into standard care.
Translating Preclinical Findings into Clinical Practice
While animal studies provide the nitty-gritty details and reveal hidden complexities of herbal interventions, translating these findings to clinical practice remains a major challenge. Healthcare providers, researchers, and regulatory bodies must work together to design robust clinical trials that reflect real-world scenarios and patient diversity. Without such studies, the application of herbal medicine will continue to be seen as a complementary, rather than a stand-alone, treatment modality.
An interdisciplinary approach—combining insights from traditional medicine, modern pharmacology, microbiology, and clinical practice—will be essential to safely and effectively introduce these therapies into mainstream medicine. By embracing both modern technology and time-tested natural remedies, we can better figure a path through the confusing bits and complicated pieces of gastrointestinal treatment.
Conclusion: Steering Through the Twists and Turns of Gastrointestinal Health
The management of functional gastrointestinal disorders is truly a multifaceted challenge laden with nerve-racking twists and turns. The recent comparative study of the herbal formulas SST and YJT shines a spotlight on how carefully crafted herbal remedies may offer a natural and effective alternative to conventional synthetic drugs. With SST showing promising effects on GI motility and hormonal regulation, and YJT providing robust enteroprotection and microbial balance, there is reason for cautious optimism among healthcare professionals looking to diversify treatment options.
However, it is important to acknowledge that the evidence is still in its early stages. Further research—especially rigorous clinical trials—is needed to fully understand the long-term safety, optimal dosing, and precise mechanisms by which these herbal remedies work. In the meantime, clinicians must remain aware of the small distinctions in patient responses and the potential interactions between herbal compounds and the unique gut microbiota of each individual.
From rethinking dosage protocols to integrating microbiota analysis, and from ensuring standardized extraction methods to educating patients on realistic outcomes, the road to adopting herbal medicine in gastrointestinal health is full of challenging yet captivating parts. As we continue to poke around and get into the hidden complexities, the hope is that natural remedies will one day match or even surpass synthetic drugs in ensuring a higher quality of life for patients with dyspepsia and other GI disorders.
This emerging field, which marries traditional knowledge with modern science, could transform the way we address functional gastrointestinal disorders. By focusing on the essential parameters—gastric motility, mucosal integrity, hormone regulation, and microbial balance—we can make a real difference. While the hurdles are many and the details may sometimes seem overwhelming, the potential benefits for patient care are super important and truly promising.
In closing, the journey towards integrating herbal solutions into mainstream healthcare is one that demands collaboration, innovative research, and a careful balancing of tradition and modernity. With continued effort, these natural therapies might soon provide a safe, effective, and holistic approach to managing the maze of gastrointestinal disorders.
Ultimately, patients and clinicians alike deserve treatments that are not only effective but also gentle on the body—offering relief from the scary side effects often seen with conventional drugs. As we continue to figure a path through this complex landscape, herbal medicine stands out as a beacon of hope amid the tangled issues of current GI treatments.
Originally Post From https://www.nature.com/articles/s41598-025-15574-9
Read more about this topic at
Regulation of Gut Microbiota by Herbal Medicines
Gut microbial modulation by culinary herbs and spices